Barriers to Exercise in Type 2 DM Patients: An Institutional Cross-Sectional Descriptive Study
Barriers to Exercise in Type 2 DM Patients: An Institutional Cross-Sectional Descriptive Study
A B S T R A C T
Background: The benefits of regular exercise are well recognized in type 2 diabetes subjects. However, a substantial proportion of patients don’t exercise at all. We aimed to enumerate the barriers to exercise in Type 2 Diabetes Mellitus (T2DM) patients and factors associated with these barriers.
Methodology: We conducted a cross-sectional study of successive type 2 diabetes patients attending routine out-patient diabetes clinics in five tertiary care hospitals in Kolkata, India from 1st April,2017 to 31st March 2018. All patients who matched our study eligibility criteria were interviewed by diabetes care providers using a structured questionnaire modeled after a systematic review of similar studies but tuned to regional preferences. Besides demographic details, patient particulars and laboratory investigations, the questionnaire included 2 direct questions on possible barriers to exercise. The questions were grouped into five categories viz. environmental (4 questions), behavioral (9 questions), occupational (2 questions), physical inability (7 questions) and medical reason (1 question). Patients’ who didn’t meet the ADA-EASD recommended exercise (at least 150 minutes moderate intensity aerobic physical activity viz. brisk walking at 3-4 km-hr) were classified as non-exercisers.
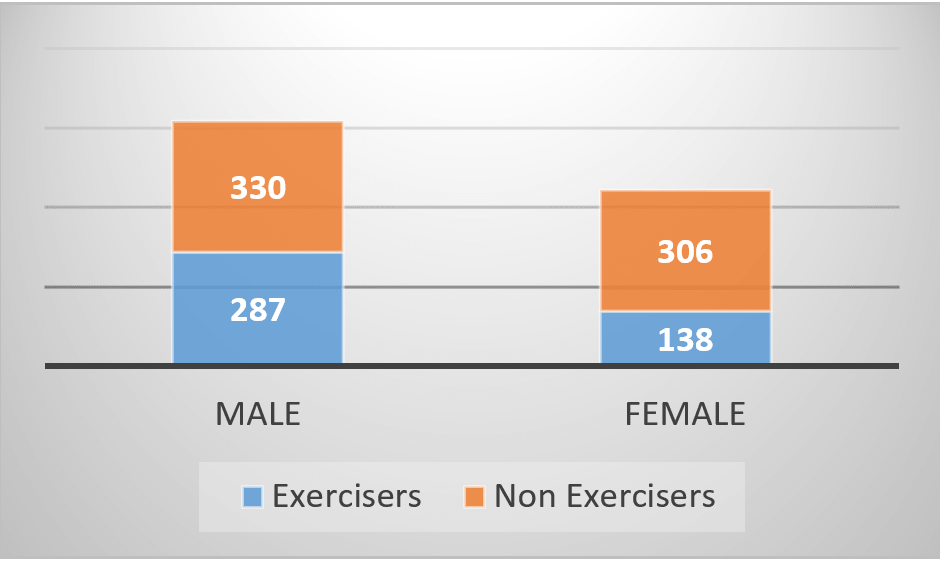
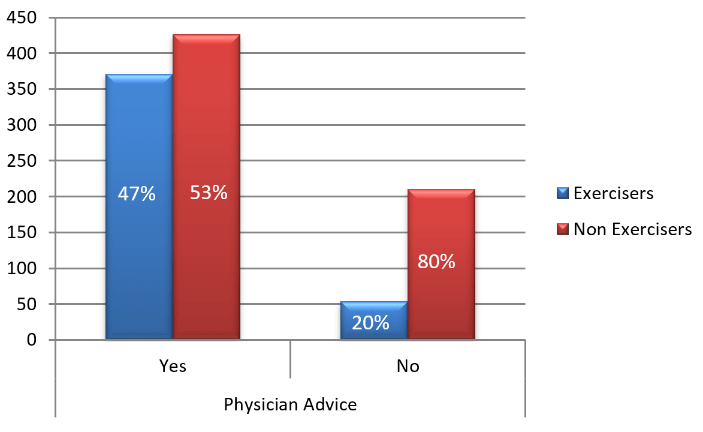
Results: The present study included a total of 1061 patients of which 617 were males versus 444 females. 636 (59.9%) were not doing physical activity as per current international standards. A substantial higher proportion of females (68.9%) did not exercised as compared to males (53.5%), which is statistically significantly higher, p<0.001. Insulin usage was found to be significantly associated to hamper exercise (p=0.017), physical activity being 8% lower (34.5% in insulin users versus 42.5% in non-insulin users). Male gender (OR-1.877, 95% CI=1.217-2.894, p=0.004) and doctor’s prior advice for exercise (OR-3.397, 95% CI=2.035-5.671, p<0.001) were found as significant predictors for increased physical activity.
Conclusion: This study elaborates the need for awareness regarding possible barriers when counseling T2DM patients. Exercise remains one of the cheapest pillars of DM management, the benefits of which extend beyond glycemic control. However, as this study illustrates about 60% of patients with T2DM do not carry out the recommended exercise. This study also highlights the importance of physician advice regarding exercise. Behavioural causes seem to be the commonest barrier to exercise and hence strategies to target the same needs to be thought of.
Keywords
Diabetes, barriers, exercise, india
Introduction
Diabetes Mellitus has assumed epidemic proportions with current prevalence estimated at 9% of which India has a staggering 66 million cases [1, 2]. Despite several medications currently available, lifestyle changes including exercise and diet remains the cornerstone of diabetes management. Exercise regimens have been associated with a reduction in HbA1c of at least 0.66% in type 2 diabetes patients in spite of unchanged BMI [3]. According to ADA/AESD guidelines, patients at risk, pre-diabetics or under treatment would significantly benefit from at least 150 min/week of moderate physical activity such as walking [4]. Unfortunately, many patients do not do the required amount of exercise. This may partly be due to lack of knowledge or a result of absence of physician’s advice in addition, there may be multiple disparate barriers to this quintessential self-care behavior in diabetes [5].
Studies aimed at finding these barriers to exercise are scarce, especially in the Asian subcontinent. Moreover, most of the available studies have targeted a small population of patient with DM [6]. With that in mind, this study was devised with a goal to describe the possible barriers to exercise, in an Indian context.
I Objectives/Aims
1. To enumerate the barriers to exercise in Type 2 Diabetes Mellitus (T2DM) patients.
2. To enumerate the relationship of the most common barriers to age, sex, lifestyle and duration of diabetes.
II Research Design & Methodology
All patients attending the Diabetes clinic in five tertiary care hospitals in Kolkata, India during the time 1st April, 2017 to 31st March 2018 were approached. Exclusion criteria included: (i) Refusal to provide written informed consent (ii) Pre-existing physical disability requiring long-term support (iii) Type 1 Diabetes Mellitus (iv) Pregnancy (v) Patients below age of eighteen (vi) Recent hospital admission for any cause within the last 6 months (vii) Any documented psychiatric illness likely to impair judgment
Consecutive patients attending diabetes clinic in the hospitals were approached and briefed about the study. Following written informed consent, willing candidates fulfilling our criteria were interviewed by diabetes care providers using a structured questionnaire available in English, Bengali and Hindi (Annexe-1). The questionnaire was devised from but not limited to a systematic review of similar studies tailoring it to circumstances relevant to our regional population [6]. They were offered 23 direct questions on possible barriers to exercise. The responses were grouped into 5 categories viz. (i) Environmental (4 question) (ii) Behavioral (9 question) (iii) Occupational (2 question) (iv) Physical Inability (7 question) (v) Medical reasons (1 question)
The questionnaire also included demographic details, patient particulars (BMI, duration of T2DM, Insulin or anti-hypertensive use) and recent laboratory investigations (HbA1c, Fasting and Postprandial glucose levels). Patients who did not meet the specified criteria for recommended exercise (at least 150 min of moderate intensity aerobic physical activity per week. e.g. brisk walking @ 3-4 Km/Hour) were classified as non-exercisers.
III Statistical Methods
Descriptive statistical analysis has been carried out in the present study. Significance is assessed at a level of 5%. Multivariate binary logistic regression was performed to find out the different independent predictors for not performing exercise after adjustment of other variables.
IV Statistical software
The Statistical software namely SAS (Statistical Analysis System) version 9.2 for windows, SAS Institute Inc. Cary, NC, USA and Statistical Package for Social Sciences (SPSS Complex Samples) Version 21.0 for windows, SPSS, Inc., Chicago, IL, USA were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs and tables.
V Results & Discussion
A total of 1061 patients were included in our study. The demographic and patient profile are shown in (Table1). The data on recent (within 3 months) HbA1C, Fasting Blood Sugar and Post Prandial Blood Sugar were available in only 624, 935 and 793 patients respectively.
Table 1: Study Sample Characteristics
|
Sex |
Male |
58.15% |
Mean HbA1c |
7.58±1.56 % |
|
Female |
41.85% |
|||
|
Mean Age |
56.23±11.61 years |
Mean Duration of DM |
9.98±8.05 years |
|
|
Mean BMI |
25.07±4.38 |
On Insulin |
30.07% |
|
|
Mean FBS |
141.6±52.9 mg/dL |
On Anti-Hypertension Drugs |
56.64% |
|
|
Mean PPBS |
190.11±80.57 mg/dL |
Exercisers |
40.06% |
|
Figure 1 : Exercise in male vs. female population
Irrespective of the various age groups, duration of diabetes, insulin uses and presence of hypertension, approximately 60% were not exercising as highlighted in (table 2).
Table 2: Exercise habits across different age groups, duration of DM, Insulin and Anti Hypertensive use
|
|
n= |
Exercise (%) |
||
|
Yes |
No |
|||
|
Age (in years) |
<40 |
89 |
38.2 |
61.8 |
|
40-60 |
573 |
40.06 |
59.94 |
|
|
>60 |
399 |
37.59 |
62.41 |
|
|
Duration of DM (in years) |
<5 |
321 |
38.94 |
61.06 |
|
5-10 |
355 |
38.03 |
61.97 |
|
|
>10 |
385 |
42.86 |
57.14 |
|
|
Insulin use |
Yes |
319 |
34.5 |
65.5 |
|
No |
742 |
42.5 |
57.5 |
|
|
Anti-Hypertensive Drug use |
Yes |
601 |
37.94 |
62.06 |
|
No |
460 |
42.83 |
57.17 |
|
|
Mean |
|
39.09±2.51 (SD) |
60.9±2.51 (SD) |
|
Figure 2 : Effect of Physician Advice (PA) on Exercise Status of Patients
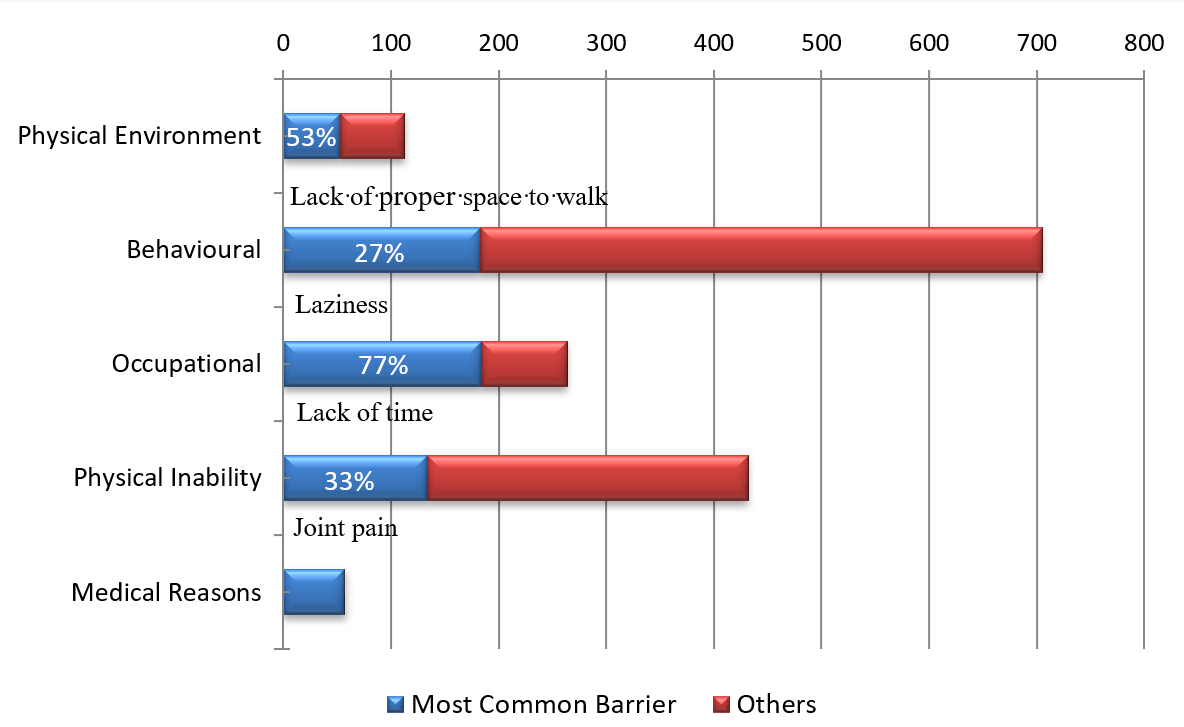
Patients who did not exercise ranked three commonest barriers to exercise applicable to them from 23 available options. It is to be noted that the respondent choice ranged from none to five in order of importance. All available responses were pooled together and grouped into 5 broad categories as outlined above. The pooled data is presented in (Table 3).
Table 3: Two most common barrier group with respect to gender, age, duration of DM and Insulin use
|
|
Most common Barrier Group |
2nd Barrier Group |
|
|
Overall |
Behavioral |
Physical Inability |
|
|
Male |
Occupational |
||
|
Female |
Physical Inability |
||
|
Age |
<60 |
Physical Inability = Occupational |
|
|
>60 |
Physical Inability |
||
|
Duration of DM (in years) |
<5 |
||
|
5-10 |
|||
|
>10 |
|||
|
Insulin use |
Yes |
||
|
No |
|||
Commonest barrier appeared to be the inability to manage time for exercise overall as well as in male patients, patients less than 60 years old, patients living with DM up to 10 years and non-insulin users. Amongst females chose joint pain as the most common barrier while patients living with DM more than 10 years and Insulin users cited laziness.
Table 4: Barriers with respect to gender, age, duration of DM and Insulin use
|
|
Barrier (in order of occurrences) |
|||||
|
Commonest |
2nd commonest |
3rd commonest |
4th commonest |
5th commonest |
||
|
Overall |
Lack of time |
Laziness |
Tiredness |
Joint Pain |
Poor sleep |
|
|
Male |
Lack of time |
Laziness |
Poor sleep |
Tiredness |
Odd office/duty hours |
|
|
Female |
Joint Pain |
Laziness |
Lack of time |
Tiredness |
Leg Cramps |
|
|
Age |
<60 |
Lack of time |
Laziness |
Poor sleep |
Tiredness |
Odd office/duty hours |
|
>60 |
Laziness |
Joint Pain |
Tiredness |
Leg Cramps |
Lack of time |
|
|
Duration of DM (in years) |
<5 |
Lack of time |
Laziness |
Tiredness |
Joint Pain |
Poor sleep |
|
5-10 |
Lack of time |
Laziness |
Joint Pain |
Poor sleep |
Tiredness |
|
|
>10 |
Laziness
|
Tiredness |
Lack of time |
Poor sleep |
Joint Pain |
|
|
Insulin use |
Yes |
Laziness |
Tiredness |
Leg Cramps |
Lack of time |
Poor sleep |
|
No |
Lack of time |
Laziness |
Joint Pain |
Tiredness |
Poor sleep |
|
Figure 3 : shows the distribution of Barrier groups and the most common barrier in that group.
The most cited barrier as the primary reason was again, difficulty to manage time for completing the recommended exercise (20%), followed by laziness/ (14%), joint pain (12%), medical reasons (9%) and joint pain (7%). The detailed break-ups are given in (Table 4) and (Figure 3).
Table 5: Multivariate logistic regression analyses of the presence of exercise as the dependent variable in our study subjects with type 2 diabetes
|
Variable |
Odds ratio of exercise (95% confidence interval) |
|||
|
|
Multivariate OR |
95% CI lower bound |
95% CI upper bound |
p |
|
Age |
.988 |
.969 |
1.009 |
.260 |
|
Sex (Male vs. Female) |
1.877 |
1.217 |
2.894 |
.004 |
|
BMI |
.951 |
.902 |
1.003 |
.063 |
|
Duration of Diabetes |
1.011 |
.980 |
1.043 |
.488 |
|
HbA1c |
1.019 |
.864 |
1.202 |
.825 |
|
FBS |
.997 |
.990 |
1.003 |
.296 |
|
PPBS |
1.000 |
.996 |
1.003 |
.823 |
|
Insulin Usage |
.568 |
.339 |
.954 |
.033 |
|
Anti-HTN Usage |
.928 |
.604 |
1.425 |
.731 |
|
Doctor Advice for exercise |
3.377 |
2.425 |
5.671 |
<0.001 |
Discussion
Although studies highlighting barriers to exercise in T2DM come up from time to time, to our knowledge this is one of the largest studies addressing the barriers to exercise in T2DM patients. Approximately 40% of the population was getting recommended exercise. In fact, about 60% patients were not exercising irrespective of their differences with respect to irrespective of age, duration of DM, Insulin or anti-hypertensive drug use. The percentage was higher among females (68.91%) and insulin users (65.52%).While inability to manage time for exercise, the most commonly cited reason (184 out of 1061) overall, belonged to the occupational group, it was the behavioral barriers that were cited more frequently (705 times). Behavioral barriers remained the most frequent barrier amongst gender, age group, duration of DM and Insulin use sub-groups. Interestingly, joint pain was cited most frequently among the females (87 out of 444) and elderly population chose laziness (77 out of 399) as the primary cause as opposed to not managing time in rest of the groups.
The present study is the first of its kind to enlighten on the perceived barriers to exercise in the Indian population. Our study results confirm that physical activity levels are low in the Indian T2DM diabetes population, with only 40.1% of patients performing physical activity as per the recommended standards. A large proportion of patients, particularly the female patients are not exercising to meet the minimum standards as per the current recommendations. In a published study by Thomas et al., which studied both type 1 and type 2 diabetes patients, only a meager 34% of patients were found to perform physical activity [7]. In addition, the authors observed a greater tendency for weight gain in inactive patients with T2DM, but in direct contrast to the findings from our study, the difference was not statistically significant. It is worth mentioning that the BMI of the physically active cohort in our study was significantly lower than the physically inactive individuals, specifically in the females but not in males. In this regard, the results of our study are in line with the previous study findings and it reveals no improvement than the UK and US based studies published ten to twenty years ago [8, 9].
One of the significant findings of our study is the remarkable benefits with regards to weight and glycemic profile observed only in the females but not males, even though significantly higher proportion of males were physically active than females. Reported barriers to physical activity were diverse in our patients but lack of time, lack of motivation, tiredness, joint pain and poor sleep were the commonest reported major barriers to exercise, and are, therefore, the main issues that needs to be addressed when seeking to enhance exercise levels in our study population. A previous study by Mier et al. in Mexican American subjects described similar common barriers to exercise namely lack of time, depression, physical pain [10].
In the similar theme, Dutton et al. tried to assess barriers to physical activity in preponderantly low-income African American T2DM subjects. As the case in our study, the most common barriers that were reported included pain and lack of time [11]. The associations we came upon between patient demographics and other patient related factors and the specific barriers to exercise reported were interesting and have the potential to allow for a tailored approach to improving adherence to exercise guidelines. Based on our results, we also recommend that patients should specifically avoid doing exercise in an empty stomach and if they do so, they must have an immediate source of carbohydrate to tackle any eventual hypoglycemia.
Another interesting finding from our study is the fact that physical activity is significantly lower among the insulin users due to the perceived fear of hypoglycemia. Hence, this patient subgroup should be trained to manage hypoglycemia when it is mild or moderate and if severe, a detailed instruction should be given. They should be educated regarding self monitoring of blood glucose, carrying glucometer when required and have an immediate source of carbohydrate while exercising. The most significant finding from our study is the fact that treating physician’s advice for exercise was positively associated with performing exercise (46.5% of patients vs. 20.5% without advice performed exercise as per the current standards; P <0.001).
I Limitations of the present study
The drawback of this study includes the fact that most of the patients were from an urban/semi urban area, therefore lacking representation from rural areas. All the patients did not have HbA1C done at the time of survey and hence correlation of exercise with good glycemic control could not be done.
II Strength of the present study
On the other hand, the interview-based design ensured more complete response for this study. Participants were offered the chance to discuss the questionnaire with the care providers before they filled in the form. This gave the educators and physicians a chance to integrate the study within the scope of their routine counseling and identify those who did not exercise, particularly clarifying recommendations. Absence of a validated questionnaire prompted us to select the barriers from existing literature and modifying them to our local population. This emphasizes the need of such a tool in evaluating the barriers in subsequent studies.
Conclusion
This study elaborates the need for awareness regarding possible barriers when counseling T2DM patients. To the best of our knowledge, this is the largest study enumerating the barriers to exercise in patients with T2DM. Exercise remains one of the cheapest pillars of DM management, the benefits of which extend beyond glycemic control. However, as this study illustrates about 60% of patients with T2DM do not carry out the recommended exercise. This study also highlights the importance of physician advice regarding exercise. Behavioral causes seem to be the commonest barrier to exercise and hence strategies to target the same needs to be thought of.
Funding
Funded by Integrated Diabetes & Endocrinology Academy, Kolkata, India.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 05, Jul 2019Accepted: Fri 26, Jul 2019
Published: Tue 03, Sep 2019
Copyright
© 2023 S. Majumdar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDMC.2019.01.01
Author Info
K.K. Gangopadhyay N. Chowdhuri A. Majumder B. Ghoshdastidar Kingshuk Bhattacharjee S. Dasgupta S. Majumdar
Corresponding Author
S. MajumdarPeerless Hospital, Department of Endocrinology and Diabetes, Kolkata, India
Figures & Tables
Table 1: Study Sample Characteristics
|
Sex |
Male |
58.15% |
Mean HbA1c |
7.58±1.56 % |
|
Female |
41.85% |
|||
|
Mean Age |
56.23±11.61 years |
Mean Duration of DM |
9.98±8.05 years |
|
|
Mean BMI |
25.07±4.38 |
On Insulin |
30.07% |
|
|
Mean FBS |
141.6±52.9 mg/dL |
On Anti-Hypertension Drugs |
56.64% |
|
|
Mean PPBS |
190.11±80.57 mg/dL |
Exercisers |
40.06% |
|
Table 2: Exercise habits across different age groups, duration of DM, Insulin and Anti Hypertensive use
|
|
n= |
Exercise (%) |
||
|
Yes |
No |
|||
|
Age (in years) |
<40 |
89 |
38.2 |
61.8 |
|
40-60 |
573 |
40.06 |
59.94 |
|
|
>60 |
399 |
37.59 |
62.41 |
|
|
Duration of DM (in years) |
<5 |
321 |
38.94 |
61.06 |
|
5-10 |
355 |
38.03 |
61.97 |
|
|
>10 |
385 |
42.86 |
57.14 |
|
|
Insulin use |
Yes |
319 |
34.5 |
65.5 |
|
No |
742 |
42.5 |
57.5 |
|
|
Anti-Hypertensive Drug use |
Yes |
601 |
37.94 |
62.06 |
|
No |
460 |
42.83 |
57.17 |
|
|
Mean |
|
39.09±2.51 (SD) |
60.9±2.51 (SD) |
|
Table 3: Two most common barrier group with respect to gender, age, duration of DM and Insulin use
|
|
Most common Barrier Group |
2nd Barrier Group |
|
|
Overall |
Behavioral |
Physical Inability |
|
|
Male |
Occupational |
||
|
Female |
Physical Inability |
||
|
Age |
<60 |
Physical Inability = Occupational |
|
|
>60 |
Physical Inability |
||
|
Duration of DM (in years) |
<5 |
||
|
5-10 |
|||
|
>10 |
|||
|
Insulin use |
Yes |
||
|
No |
|||
Table 4: Barriers with respect to gender, age, duration of DM and Insulin use
|
|
Barrier (in order of occurrences) |
|||||
|
Commonest |
2nd commonest |
3rd commonest |
4th commonest |
5th commonest |
||
|
Overall |
Lack of time |
Laziness |
Tiredness |
Joint Pain |
Poor sleep |
|
|
Male |
Lack of time |
Laziness |
Poor sleep |
Tiredness |
Odd office/duty hours |
|
|
Female |
Joint Pain |
Laziness |
Lack of time |
Tiredness |
Leg Cramps |
|
|
Age |
<60 |
Lack of time |
Laziness |
Poor sleep |
Tiredness |
Odd office/duty hours |
|
>60 |
Laziness |
Joint Pain |
Tiredness |
Leg Cramps |
Lack of time |
|
|
Duration of DM (in years) |
<5 |
Lack of time |
Laziness |
Tiredness |
Joint Pain |
Poor sleep |
|
5-10 |
Lack of time |
Laziness |
Joint Pain |
Poor sleep |
Tiredness |
|
|
>10 |
Laziness
|
Tiredness |
Lack of time |
Poor sleep |
Joint Pain |
|
|
Insulin use |
Yes |
Laziness |
Tiredness |
Leg Cramps |
Lack of time |
Poor sleep |
|
No |
Lack of time |
Laziness |
Joint Pain |
Tiredness |
Poor sleep |
|
Table 5: Multivariate logistic regression analyses of the presence of exercise as the dependent variable in our study subjects with type 2 diabetes
|
Variable |
Odds ratio of exercise (95% confidence interval) |
|||
|
|
Multivariate OR |
95% CI lower bound |
95% CI upper bound |
p |
|
Age |
.988 |
.969 |
1.009 |
.260 |
|
Sex (Male vs. Female) |
1.877 |
1.217 |
2.894 |
.004 |
|
BMI |
.951 |
.902 |
1.003 |
.063 |
|
Duration of Diabetes |
1.011 |
.980 |
1.043 |
.488 |
|
HbA1c |
1.019 |
.864 |
1.202 |
.825 |
|
FBS |
.997 |
.990 |
1.003 |
.296 |
|
PPBS |
1.000 |
.996 |
1.003 |
.823 |
|
Insulin Usage |
.568 |
.339 |
.954 |
.033 |
|
Anti-HTN Usage |
.928 |
.604 |
1.425 |
.731 |
|
Doctor Advice for exercise |
3.377 |
2.425 |
5.671 |
<0.001 |
References
- WHO | Diabetes (2015) World Health Organization.
- Shaw JE, Sicree RA, Zimmet PZ (2010) Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 87: 4-14. [Crossref]
- Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT et al. (2011) Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA 305: 1790-1799. [Crossref]
- American Diabetes Association (2014) Standards of medical care in diabetes--2014. Diabetes Care 37: 14-80. [Crossref]
- Walsh JM, Swangard DM, Davis T, McPhee SJ (1999) Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med 16: 307-313. [Crossref]
- Korkiakangas EE, Alahuhta MA, Laitinen JH (2009) Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: A systematic review. Health Promot Int 24: 416-427. [Crossref]
- Thomas N, Alder E, Leese GP (2004) Barriers to physical activity in patient with diabetes. Postgrad Med J 80: 287-291. [Crossref]
- Ford ES, Herman WH (1995) Leisure-time physical activity patterns in the US diabetic population. Findings from the 1990 National Health Interview Survey--Health Promotion and Disease Prevention Supplement. Diabetes Care 18: 27-33. [Crossref]
- Nelson KM, Reiber G, Boyko EJ (2002) Diet and exercise among adults with type-2 diabetes findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care 25: 1722-1728. [Crossref]
- Mier N, Medina AA, Ory MG (2007) Mexican Americans with type 2 diabetes: perspectives on definitions, motivators and programs of physical activity. Prev Chronic Dis 4: A24. [Crossref]
- Dutton GR, Johnson J, Whitehead D, Bodenlos JS, Brantley PJ (2005) Barriers to physical activity among predominantly low-income African-American patients with type 2 diabetes. Diabetes Care 28: 1209-1210. [Crossref]
