Association Between Cervical Length at 18-23 Weeks of Gestation and Spontaneous Preterm Delivery: A Cross Sectional Study
A B S T R A C T
Introduction: Preterm birth is childbirth occurring at less than 37 completed weeks or 259 days of gestation, is a major determinant of neonatal mortality and morbidity and has long-term adverse consequences for health. Identifying ways to address preventable causes of preterm birth should be a top priority in developing regions of the world. the present study was planned to find the association between cervical length at 18 to 23 weeks of gestation done as a routine during all second level scans and spontaneous preterm delivery.
Patients and Methods: This is a hospital based cross sectional study conducted during the period from January 2019 to December 2019. A total of 205 women presenting with singleton pregnancies between 18-23 weeks of gestations were assessed by transvaginal ultrasound for the measurement of cervical length. Patients were interviewed and their demographic data such as age, obstetric index(GPALD), obstetric history such last menstrual period (LMP), estimated delivery date (EDD) and current pregnancy details such as BP, pulse rate, pallor, period of gestation, were recorded in a predesigned pro forma.
Results: In a total of 205 subjects, the average age was found to be 23.26 ± 3.49 years with 52.2% of the women being primigravida. The mean gestation age at the time of enrollment was 20.72 ± 1.00 weeks with 33% of women showing a cervical length of 26-30 mm. The delivery outcome was found as 11% preterm, majority (89.27%) was term delivery.
Conclusion: The present study showed that a significantly higher number of women with cervical length ≤ 30 mm (assessed at 18 to 23 weeks of gestation) had preterm labour compared to a woman with cervical length > 30 mm.
Keywords
Cervical length, preterm birth, childbirth and morbidity
Introduction
Preterm birth is childbirth occurring at less than 37 completed weeks or 259 days of gestation, is a major determinant of neonatal mortality and morbidity and has long-term adverse consequences for health [1-3]. If preterm labor leads to an early delivery, the premature newborn is at risk for problems related to incomplete development of its organ systems. Children who are born prematurely have higher rates of cerebral palsy, sensory deficits, learning disabilities and respiratory illnesses compared with children born at term. The morbidity associated with preterm birth often extends to later life, resulting in enormous physical, psychological and economic costs [4, 5].
Preterm delivery is the main cause of perinatal mortality and morbidity [6]. Spontaneous preterm birth occurs before 37 weeks’ gestation in 7-11% of pregnancies, and before 34 weeks’ gestation in 3-7% of pregnancies [6, 7]. Delivery before 34 weeks’ gestation, however, accounts for three-quarters of neonatal mortality and one half of long-term neurological impairment in children. The incidence of preterm labour in our institute during 2006-2007 was reported to be 10.2% and of these, 50% occurred spontaneously and preterm premature rupture of membrane (PPROM) and iatrogenic causes contributed 25% each [8].
Clearly, different risk factors play a role in the high rates of preterm birth in different regions. In North America, the increasing age of women giving birth, which leads to more maternal complications and Caesarean sections, may partially explain the high rates. Increased rates of multiple pregnancies may be another explanation. In Africa, on the other hand, high levels of preterm birth are probably due to intrauterine infection or lack of availability of drugs, such as tocolytic agents [9]. However, two main factors contribute to such disappointing figures: (1) the inadequacy of therapeutic arsenal; indeed, only tocolytics attempt to treat symptoms of preterm labor; (2) the absence of reliable criteria for the selection of a high-risk population for preterm delivery [10].
Hence, identifying ways to address preventable causes of preterm birth should be a top priority in developing regions of the world. Despite the advances in the diagnosis and management of preterm labour, prediction of preterm labour is issue of debate as to large extent the preterm labour cannot be predicted and attempts such as risk factors, fetal fibronectin, bacterial vaginosis and cervical length assessment are questionable. Considering the high rate of preterm delivery and its adverse consequences and with hypothesis that short cervical length may predict the preterm delivery, the present study was planned to find the association between cervical length at 18 to 23 weeks of gestation done as a routine during all second level scans and spontaneous preterm delivery.
Methodology
This is a hospital based cross sectional study conducted at Department of Obstetrics and Gynecology, KLE’S Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum during the period from January 2019 to December 2019 after obtaining ethical clearance. A total of 205 women presenting with singleton pregnancies between 18-23 weeks of gestations were assessed by transvaginal ultrasound for the measurement of cervical length. Exclusion criteria were multiple gestations and patient not willing to provide informed consent.
Patients were interviewed and their demographic data such as age, obstetric index(GPALD), obstetric history such last menstrual period (LMP), estimated delivery date(EDD) and current pregnancy details such as BP, pulse rate, pallor, period of gestation, were recorded in a predesigned pro forma. Further these women were subjected to transvaginal ultrasound using a Philips HD 11 ultrasound machine and a vaginal probe of 8 MHz [11]. The probe was placed in the anterior fornix of the vagina without exerting undue pressure on the cervix, which may artificially elongate the cervix. The image was magnified. A sagittal view of the cervix was obtained. The calipers were used to measure the linear distance between the triangular area of echodensity at the external os and the V shaped notch at the internal os. Three measurements were taken over a period of 3 minutes to observe any dynamic changes in cervix, and the least of the three measurements was considered. All the patients were followed up till delivery, to assess the outcome of the pregnancy such as gestational age at delivery, perinatal details, delivery outcome(term/preterm), birthweight and of delivery mode .
Chi-square test and unpaired two sample ‘t’ test with unequal variance were conducted to analyse the data at 95% confidence limits. In the analysis, the categorical data was expressed as rates, ratios and proportions and continuous data was expressed as mean ± standard deviation (SD). The results were considered for statistical significance at 5%.
Results
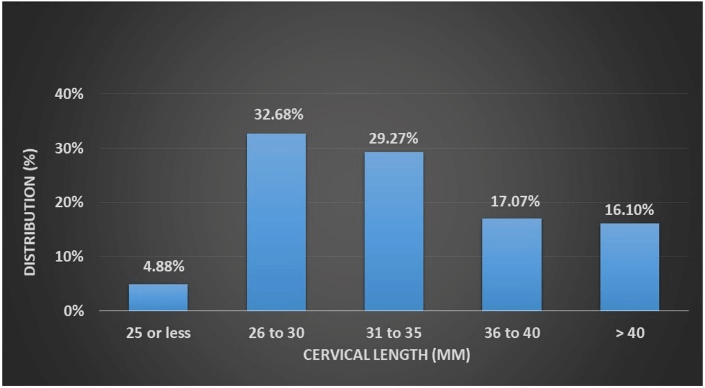
In a total of 205 subjects, the average age was found to be 23.26 ± 3.49 years with 52.2% of the women being primigravida. The mean gestation age at the time of enrollment was 20.72 ± 1.00 weeks with 33% of women showing a cervical length of 26-30 mm. Figure 1 shows distribution of women with varying cervical lengths from <25mm to >4omm. The delivery outcome was found as 11% preterm; however, majority (89.27%) was term delivery. Figure 2 depicts the distribution of varying Cervical lengths and the delivery outcome.
Figure 1: Distribution of women with varying cervical lengths from <25mm to >4omm.
Figure 2: Distribution of varying cervical lengths and the delivery outcome.
Figure 3: Mean cervical length - Term/Preterm delivery.
The above graph shows that out of the 10 babies delivered by the mothers with cervical length ≤ 25 mm 50% were preterm compared to 11.27% with cervical length 26 to 30 mm, 5.36% with 31 to 35 mm, 14.29% with 36 to 40 mm and 3.03% with cervical length of > 40 mm. This difference was statistically significant (p=0.003). Table 1 shows the association between Mean cervical length and delivery outcome and (Figure 3) depicts the same. In this study the mean cervical length of the mothers who gave birth to preterm babies was significantly less (29.64 ± 8.73 mm) compared to those who delivered term babies (34.16 ± 5.72 mm) (p=0.002). In this study 52.2% of the women were primigravida while 27.8% and 20% were gravida 2 and 3 or more respectively. Majority (76.59%) of the women were enrolled between 20 to 21 weeks’ gestation. The mean gestation at enrollment was 20.72 ± 1.00 weeks. In this study the fundal height at enrollment corresponded to 20 weeks in 79.02% of women and to 22 weeks and 24 weeks in 15.12% and 5.85% respectively. The mean fundal height was noted as 20.41 ± 1.02 weeks. 32.68% of the women had cervical length between 26 to 30 mm while 29.27% had same between 31 to 35 mm.
Table 1: Mean Cervical length - Term/Preterm delivery.
|
|
Mean cervical length (mm) |
p value |
|||
|
Term (n=183) |
Preterm (n=22) |
||||
|
Mean |
SD |
Mean |
SD |
||
|
Mean cervical length |
34.16 |
5.72 |
29.64 |
8.73 |
0.002 |
However, cervical length of ≤ 25 mm was noted in 4.88% of women and the mean cervical length was 33.67 ± 6.24 mm. 80% of the women had vaginal delivery while 18.05% had instrumental delivery. However, LSCS delivery was noted in 1.95% of women. among 98.54% of women the pregnancy outcome was live birth. However, 0.98% of the women had IUD and 0.49% of women had fresh stillbirth. 73.66% of babies weighed between 2.50 to 3.49 Kgs. In the remaining, 20.49% had birth weight between 1.50 to 2.49 Kgs while 4.88% of babies weighed > 3.50 Kgs. The mean birth weight was 2.75 ± 0.45 Kgs. In the present study of the 22 preterm babies, 59.09% were born to mothers with cervical length ≤ 30 mm compared to 40.91% babies which were born to mothers with cervical length > 30 mm. This difference was statistically significant (p=0.027). The mean cervical length of the mothers who gave birth to preterm babies was significantly less (29.64 ± 8.73 mm) compared those who delivered term babies (34.16 ± 5.72 mm) (p=0.002). In the present study of the 10 babies delivered by the mothers with cervical length ≤ 25 mm 50% were preterm compared to 11.27% with cervical length 26 to 30 mm, 5.36% with 31 to 35 mm, 14.29% with 36 to 40 mm and 3.03% with cervical length of > 40 mm. This difference was statistically significant (p=0.003).
Discussion
Preterm birth is a major cause of perinatal morbidity and mortality, and despite improvements in perinatal management over the last two decades, the rate of preterm birth has not declined [1-8]. A number of risk factors of preterm birth have been identified, one of the most important being a history of spontaneous preterm birth. Cervical length, as measured by transvaginal ultrasonography, has been shown to predict preterm birth in asymptomatic low-risk women as well as those presenting with threatened preterm labor.
Cervical length is a better predictor of preterm birth in women at increased risk, such as those with a history of spontaneous preterm birth, than in asymptomatic women at low risk [12]. In the present study of the 22 preterm babies, significantly higher number of babies (59.09%) were born to the mothers with cervical length ≤ 30 mm compared to mother with cervical length > 30 mm (40.91%) (p=0.027). Similarly, on qualitative analysis the mean cervical length of the mothers who gave birth to preterm babies was significantly less compared those who delivered term babies (29.64 ± 8.73 mm versus 34.16 ± 5.72 mm; p=0.002). These findings suggest that a reduced cervical length is significant risk factor for the preterm delivery. Further, of the 10 babies delivered by the mothers with cervical length ≤ 25 mm 50% were preterm compared to 11.27% with cervical length 26 to 30 mm, 5.36% with 31 to 35 mm, 14.29% with 36 to 40 mm and 3.03% with cervical length of > 40 mm. This difference was statistically significant (p=0.003). These findings implicate a trend towards higher chances of preterm as the cervical length decreases.
Andersen et al. were the first to note the use of TVU in the prediction of preterm birth [13]. They reported a cervix of less than 39 mm before 30 weeks of gestation as a risk factor for early delivery. Interestingly, in several studies evaluation of the cervix was performed by TAU with an empty or nearly empty bladder, and the mean cervical lengths were similar to those detected by TVU [14-16].
Tsoi et al. reported that among 216 patients with threatened PTL, 37% of those with cervical length <15 mm delivered within 7 days, indicating an odds ratio for delivery of 101 (95% CI: 12-800; p <0.0001) [17]. The same authors found that the 25mm cut-off was the most effective in discriminating between true and false labor in twin pregnancies [11].
Another study from Jordan to determine whether transvaginal ultrasound assessment of the cervix is superior to transabdominal ultrasonography in evaluating the cervical canal in the second trimester and to see which one is more accurate in predicting preterm labor concluded that, a short cervix in the second trimester detected by ultrasound is a strong predictor of spontaneous preterm labour at all gestational age [18]. TVU seems to be superior to TAU in assessing the cervical length in the second trimester and for screening for spontaneous preterm delivery.
In studies of women with a history of preterm birth, using a cervical length cut-off of 25 to 30 mm to predict preterm birth < 37 weeks of gestation, sensitivity is 60% to 80%, positive predictive value is 55% to 70%, and negative predictive value is 89% to 94%. Thus, a long cervix (at least 25 to 30 mm) is reassuring and can help to reduce unnecessary and costly interventions, such as activity restriction, maternal transfer, steroids, and tocolytics [12].
A study from Manipal to compare the difference in the cervical length measured digitally or by transabdominal and transvaginal sonogram examination for prediction of preterm labour reported statistically significant difference in the mean length of whole cervix between control and case (those who had symptoms of premature contraction) i.e. 3.70 cm Vs 2.34cm [19]. Similar differences were observed between control and those who had preterm labour (3.62cm vs 2.30 cm). The study concluded that, TVS is a simple tool for prediction of preterm labour as decrease in cervical length was observed in women with threatened preterm labor (2.34 cm) and this decrease was statistically significant compared to that of the control (3.7 cm).
A Randomized Trial by Fonseca et al. reported a 15% absolute risk reduction of early preterm delivery for patients supplemented with vaginal progesterone, after the detection of a sonographic short cervix, these findings support a future strategy of routine cervical length screening and progesterone supplementation [20]. In the Future, when definite interventions for prevention of preterm birth are expected to be available, it would be perhaps ethically unacceptable to withhold treatment if data suggests a substantial risk. Overall, sonographic cervical length measurement proves to be a simple, effective method for screening patients at routine anomaly scan. However, as the cut of 25 mm and 30 mm both were effective in determining the preterm in this study, the further studies on large sample with standardized maternal age, period of gestation, risk factors are warranted.
Conclusion
The present study showed that a significantly higher number of women with cervical length ≤ 30 mm (assessed at 18 to 23 weeks of gestation) had preterm labour compared to a woman with cervical length > 30 mm. Further the mean cervical length of women who had preterm labour was significantly less compared to women who reached term. Also, 50% of women with cervical length ≤ 25 mm delivered preterm babies. Based on these results, it may be concluded that, there is an association between short cervical length (≤ 30 mm) and spontaneous preterm delivery.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 19, Oct 2020Accepted: Thu 29, Oct 2020
Published: Tue 24, Nov 2020
Copyright
© 2023 Trupti Ruge. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CROGR.2020.03.02
Author Info
Corresponding Author
Trupti RugeDepartment of Gynecology and Obstetrics, Navodaya Medical College, Raichur, India
Figures & Tables
Table 1: Mean Cervical length - Term/Preterm delivery.
|
|
Mean cervical length (mm) |
p value |
|||
|
Term (n=183) |
Preterm (n=22) |
||||
|
Mean |
SD |
Mean |
SD |
||
|
Mean cervical length |
34.16 |
5.72 |
29.64 |
8.73 |
0.002 |


References
- International classification of diseases and related health problems (1992) 10th revision. Geneva: World Health Organization.
- Huddy CL, Johnson A, Hope PL (2001) Educational and behavioral problems in babies of 32-35 weeks’ gestation. Arch Dis Child Fetal Neonatal Ed 85: 23F-28F. [Crossref]
- Wang ML, Dorer DJ, Fleming MP, Catlin EA (2004) Clinical outcomes of near-term infants. Pediatrics 2004 114: 372-376. [Crossref]
- Petrou S (2005) The economic consequences of preterm birth during the first 10 years of life. BJOG 112: 10-15. [Crossref]
- Petrou S, Mehta Z, Hockley C, Cook Mozaffari P, Henderson J et al. (2003) The impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics 112: 1290-1297. [Crossref]
- Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM et al. (2002) Births: final data for 2002. Natl Vital Stat Rep 51: 1-102. [Crossref]
- Maternal and Child Health Research Consortium (MCHRC) (1997) Confidential Enquiries into Stillbirths and Deaths in Infancy (CESDI): 6th Annual Report. London: MCHRC.
- Honest H, Bachmann LM, Coomarasamy A, Gupta JK, Kleijnen J et al. (2003) Accuracy of cervical transvaginal sonography in predicting preterm birth: a systematic review. Ultrasound Obstet Gynecol 22: 305-322. [Crossref]
- Romero R, Espinosa J, Mazor M, Chaiworapongsa T (2004) The preterm parturition syndrome. In: Critchley H, Bennett P, Thornton S, eds. Preterm birth. London: RCOG Press.
- Rozenberg P, Gillet A, Ville Y (2002) Transvaginal sonographic examination of the cervix in asymptomatic pregnant women: review of the literature. Ultrasound Obstet Gynecol 19: 302-311. [Crossref]
- Fuchs I, Tsoi E, Henrich W, Dudenhausen JW, Nicolaides KH (2004) Sonographic measurement of cervical length in twin pregnancies in threatened preterm labor. Ultrasound Obstet Gynecol 23: 42-45. [Crossref]
- Lim K, Butt K, Crane JM (2011) SOGC Clinical Practice Guideline. Ultrasonographic cervical length assessment in predicting preterm birth in singleton pregnancies. J Obstet Gynaecol Can 33: 486-499. [Crossref]
- Andersen HF, Nugent CE, Wanty SD, Hayashi RH (1990) Prediction of risk for preterm delivery by ultrasonographic measurement of cervical length. Am J Obstet Gynecol 163: 859-867. [Crossref]
- Zemlyn S (1981) The length of the uterine cervix and its significance. J Clin Ultrasound 9: 267-269. [Crossref]
- Bowie JD, Andreotti RF, Rosenberg ER (1983) Sonographic appearance of the uterine cervix in pregnancy. AJR Am J Roentgenol 140: 737-740. [Crossref]
- Varma TR, Patel RH, Pillai U (1986) Ultrasonographic assessment of cervix in normal pregnancy. Acta Obstet Gynecol Scand 65: 229-233. [Crossref]
- Gramellini D, Fieni S, Kaihura C, Modena AB (2007) Cervical length as a predictor of preterm delivery: gestational age-related percentiles vs fixed cut-offs. Acta Biomed 78: 220-224. [Crossref]
- Rashed M, Rawashdeh M, Be Kaen K (2009) Prediction of preterm labor by ultrasonographic cervical length. RMJ 34: 191-194.
- Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH (2007) Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med 357: 462-469. [Crossref]
- Tsoi E, Akmal S, Rane S, Otigbah C, Nicolaides KH (2003) Ultrasound assessment of cervical length in threatened preterm labor. Ultrasound Obstet Gynecol 21: 552-555. [Crossref]
