Antibacterial Drugs Utilization among Patients Admitted to Medical Wards of Magway Regional Hospital
A B S T R A C T
Background: Drug utilization studies are important elucidation tools for prescribing habits in particular therapeutic field and they play a key role in helping the healthcare personnel to understand, interpret and improve the prescribing, administration and use of medications.
Objectives: This study was undertaken to identify amount of antibacterial drugs used and utilization patterns of antibacterial drugs in medical wards of Magway Regional Hospital.
Methods: This study is a hospital-based, cross-sectional, descriptive study and was carried out for a period of four months. Data regarding antibacterial prescription during hospital stay were collected from medical record files of patients. The data were evaluated by Microsoft Excel software.
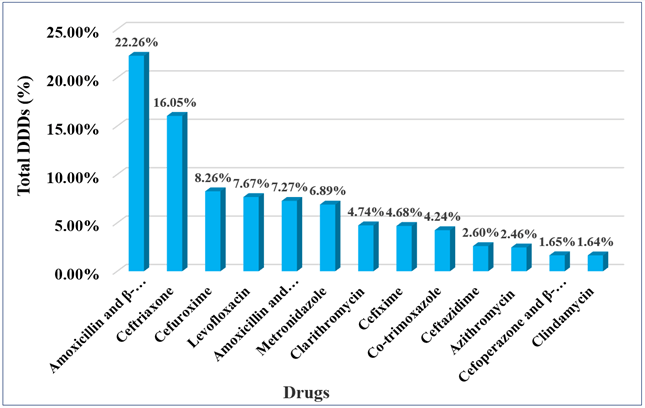
Results: In this study, the most common indications for antibacterials were respiratory tract infections (43.34%) followed by gastrointestinal tract infections (16.27%). Out of 879 patients, 52.10% were prescribed by single antibacterial agent and in 47.90%, combination of antibacterials was necessary to be given. Antibacterials were prescribed by oral route in 29.58% and parenteral route were prescribed in 29.35% while 41.07% patients received antibacterials by both oral and parenteral routes. Antibacterials were prescribed with generic name in 64% and trade name in 36%. Cephalosporins were the most commonly prescribed drugs, 68.26%, followed by penicillin groups and quinolones, 53.58% and 16.27% respectively. In this study, 13 drugs included in DU90% segment were amoxicillin and β-lactamase inhibitor combination (22.26%), ceftriaxone (16.05%), cefuroxime (8.26%), levofloxacin (7.67%), amoxicillin and flucloxacillin combination (7.27%), metronidazole (6.89%),clarithromycin (4.74%), cefixime (4.68%), co-trimoxazole (4.24%), ceftazidime (2.6%), azithromycin (2.46%), cefoperazone and β-lactamase inhibitor combination (1.65%) and clindamycin (1.64%).
Conclusions: The findings from this study will provide the documentary evidence regarding antibacterial utilization patterns in treatment of a variety of infections and antibacterial drugs include in DU90% segment. This information generally contributes data for making decision of purchasing medicines or preparing drug budgets.
Keywords
Drug utilization, antibacterial drugs, magway regional hospital
Introduction
The process of drug utilization studies focus on the factors related to prescribing, dispensing, administering and taking of medication, and its associated events, either beneficial or adverse [1]. The early work of drug utilization studies did not permit detailed comparisons of the drug utilization data obtained from different countries because the source and form of the information varied between them. To measure drug use, it is important to have both a classification system and a unit of measurement. Norwegian researchers developed a system known as Anatomical Therapeutic Chemical (ATC) classification [2].
A technical unit of measurement called the defined daily dose (DDD) to be used in drug utilization studies was developed by World Health Organization (WHO). Drug consumption data present in DDDs give a rough estimate of consumption and allow comparison of trends in drug consumption, between countries and population groups and over time [3]. Drug utilization 90% (DU90%) is focusing on the drugs that account for 90% of the prescribed volume. It can be used for international comparison of drug utilization and in feedback to prescribers, as a way of implementing guidelines [4]. The main purpose of the ATC/DDD system is to be used as a tool for presenting drug utilization statistics with the aim of improving drug use. The system has been used since the early 1970s in drug utilization studies. It is suitable for national and international comparisons of drug utilization and for the evaluation of long-term trends in drug [5].
Nowadays, infections are very common and responsible for a large number of diseases adversely affecting human health. Myanmar is one of the developing countries in the tropical region. The prevalence of infectious diseases in Myanmar is very high. Antibacterial drugs are agents that can suppress the growth of bacteria or destroy them. Use of these drugs in clinical practice has changed the natural course and improved the prognosis of infectious diseases. They are the most common group of drugs prescribed in hospital. Therefore, it is important to determine drug use pattern and drug use profile over time.
Estimation of antibacterial drugs utilization using ATC/DDD methodology will help to compare antibacterial utilization with time, between departments, hospitals and neighboring countries. The study of antibacterial drug utilization provides documentary evidence regarding prescribing patterns of antibacterial drugs. By knowing DU90%, it can help administrator for drug procurement. This information generally contributes data for making purchase decisions or preparing drug budgets.
Materials and Method
This study was hospital-based, cross-sectional descriptive study carried out in Medical wards of Magway Regional Hospital. All medical record files of patients admitted to medical wards of Magway Regional Hospital during 1st January 2016 to 30th April 2016 were reviewed and those received antibacterials were included in this study. The data collection for each patient was done from the admission to the discharge. Data regarding admission diagnosis, discharge diagnosis, duration of hospitalization, antibacterial prescription during hospital stay were recorded.
Data also included drug names, dosage, route of administration, frequency of administration and duration of drug therapy. Collected data were recorded and entered into Microsoft Excel work sheet. The data were presented in frequency and percentage table. Drugs utilization data were analyzed by using the World Health Organization (WHO) anatomical therapeutic chemical (ATC) classification/ defined daily dose (DDD) methodology. The ATC codes and DDD for each antibacterial drug were obtained from ATC index with DDDs 2016 [5]. Then the total numbers of DDDs for each antibacterial drug was calculated from the collected data by formula [3].
$$ Drug usage (DDDs) = \frac{Number\ of\ Items\ issued\ ×\ Amount\ of\ drug\ per\ item}{DDD} $$
Then DU90% segment was calculated by ranking antibacterials by volume of DDDs, summing the DDDs for these drugs and then determining how many drugs accounted for 90% of drug use. DU90% identifies the drugs accounting for 90% of the volume of prescribed drugs after ranking the drugs used by volume of DDDs.
Results
During the study period, antibacterial therapy was prescribed in 879 of total 1361 admission. Figure 1 shows distribution of diseases in study population who were prescribed antibacterials. The most common indications for antibacterial drugs prescription were respiratory infections 43.34% (381 patients) followed by gastrointestinal (GI) infections 15.13% (133 patients).
Total of 879 patients, 458 patients (52.10%) were prescribed by single antibacterial agent and in 421 patients (47.90%) were prescribed by combination therapy. Antibacterials were prescribed by oral route in 260 patients (29.58%) and parenteral route was prescribed in 258 patients (29.35%) patients while 361 patients (41.07%) patients took antibacterials by both oral and parenteral routes. Antibacterials were prescribed with generic name in 64% and trade name in 36%.
Figure 1: Distribution of diseases in study population who were prescribed antibacterials (n=879).
Figure 2: Distribution of utilization of different antibacterial groups among study population.
Figure 3: Drug Utilization 90% segment of antibacterials in medical wards of Magway Regional Hospital.
Among prescribed groups of antibacterials, cephalosporins were the most frequently prescribed drugs and it is followed by penicillin groups and quinolones as shown in (Figure 2). Figure 3 shows that the drug utilization 90% of antibacterials in Magway Regional Hospital. In this study, 13 drugs were included in DU90% segments.
Discussion
Nowadays, infections are very common and responsible for a large number of diseases affecting human health. Appropriate antimicrobial treatment greatly improves the prognosis of infectious diseases. There has been a very significant reduction in morbidity and mortality associated with the use of antimicrobial agents since they were first introduced [6].
Whenever necessary to prescribe antimicrobial agents, there are points to be considered. They include obtaining an accurate diagnosis of infection; understanding the difference between empiric and definitive therapy; susceptibility of infecting microorganism, pharmacokinetic and pharmacodynamic factors, anatomical site of infection, toxicity and host factors such as allergy history, age, renal function, hepatic function, pregnancy status, genetic or metabolic abnormalities, host defenses, need for combination therapy and antibiotic resistance concerns [7]. So, it is important to determine drug use pattern and drug use profile over time. The present study was conducted to study antibacterial drugs utilization among patients admitted to medical wards of Magway Regional Hospital from 1st January 2016 to 30th April, 2016. The World Health Organization ATC/DDD methodology and DU90% segment were applied in the present study.
Bacterial infections of the respiratory tract remain a major cause of morbidity and death in both developed and developing countries. The burden of disease falls across all age groups from young children to the elderly [8]. Aye-Thi-Khing (2013) stated that respiratory tract infections were most frequent clinical conditions for antibiotics prescribing followed by gastrointestinal infections in medical wards of Yangon General Hospital [9]. So also, in present study, respiratory tract infections were the most prevalent diagnosis among study population and gastrointestinal infections were the second most common indications for antibacterial drugs.
According to the principle of antibiotic prescription, most of the infections should be treated with single antimicrobial agent. The evidence that the combination antimicrobial therapy is of value in life-threatening infections, polymicrobial infection, empiric therapy of suspected mixed infections, preventing resistance to monotherapy, accelerating the rapidity of microbial kill and enhancing therapeutic efficacy by use of synergistic interactions [10]. In this study, single antibacterial use was 52.10% and combination therapy was 47.90%.
Patients hospitalized with infections are often treated with intravenous antimicrobial therapy because their admission is often prompted by the severity of their infection. However, patients with mild to moderate infections and have normal gastrointestinal function are candidates for treatment with well-absorbed oral antimicrobials [11]. In this study, antibacterial drugs were prescribed mostly by using both oral and parenteral route of administration. During study period, patients were prescribed antibacterials with generic name 64% and trade name 36%. Antibacterial combinations such as amoxicillin with β-lactamase inhibitor, amoxicillin with flucloxacillin and cefoperazone with β-lactamase inhibitor were prescribed with trade name. Other antibacterials were prescribed with generic name.
In this study, the most commonly prescribed antibacterial group was cephalosporin (68.26%) followed by penicillin groups (54.49%). A study in medical ward of Yangon General Hospital, cephalosporins ranked the first and more than half of study population [9]. The penicillins constitute one of the most important groups of antibacterial. Many of these have unique advantages such that members of this group of antibiotics are the drugs of choice for a large number of infectious diseases. Moreover, combination of penicillin with β lactamases inhibitors provided the wider spectrum of antibacterial actions. In this study, amoxicillin and β-lactamase inhibitor, ceftriaxone, cefuroxime, levofloxacin, amoxicillin and flucloxacillin, metronidazole, clarithromycin, cefixime, co-trimoxazole, cetazidime, azithromycin, cefoperazone and β-lactamase inhibitor and clindamycin were in DU90% segment.
Amoxicillin and β-lactamase inhibitor combination was most commonly prescribed antibiotic in 2036.5 DDDs and 22.26% of total antibacterials used. In previous study conducted in Yangon General Hospital by Aye-Thi-Khaing (2013), most frequent use antibiotic was co-amoxiclav 29.4% [9]. In 3-month, study of Han- Lin-Aung in No (2) DSGH, the most commonly used antibiotic was ciprofloxacin and co-amoxiclav. In this study, respiratory infections were most common, and this was the reason for highest use of amoxicillin and β-lactamases inhibitor combination [12]. In this study, ceftriaxone was second rank in DU 90%, 1468 DDDs and 16.05% of total antibacterials used which was frequently prescribed cirrhosis of liver, aspiration pneumonia in patient with CVA and meningitis. Ceftriaxone was uniformly involved in DU90% of other studies, study of Libya, ceftriaxone was prescribed 22.23% in Palastine hospital [13, 14].
Cefuroxime is the second most commonly used cephalosporin and third rank in DU 90% in this study. It was indicated mostly in chest infections and COPD. In this study, levofloxacin was frequently used quinolones and it was mainly used for respiratory tract infections. The result was the same with study conducted in India [15].
In this study, amoxicillin with flucloxacillin was prescribed 7.27% of total antibacterials used and second most commonly used penicillin. It was mainly used in snake bite in study population. In snake bite, antibiotics not only prevent dissemination of infection but also accelerate healing [16].
Conclusion
By studying antibiotic prescribing patterns in medical wards of Magway Regional Hospital, it would provide the documentary evidence regarding antibacterial prescription patterns in the treatment of various infections. Moreover, this documentary evidence can give some help to inform clinicians, researchers, and/or policymakers. By knowing DU 90% can help for making purchase decisions and preparing drug budgets.
Study Limitations
The first limitation that this study was done in medical wards of Magway Regional Hospital, thus the result might not be generalized to all wards of Magway Regional Hospital. In addition, this study was carried out over 4 months period, thus the prescription pattern of antibacterials might differ among different months in a year.
Acknowledgements
Firstly, the authors acknowledge all the members of the Board of Post-graduate Studies of University of Medicine, Magway for giving the opportunity to carry out this research. They also acknowledge the patients for their participation in this study, as well as the staffs of the hospital for their assistance in patient’s data collection and their colleagues for their help and advice.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 15, Feb 2020Accepted: Wed 01, Apr 2020
Published: Tue 28, Apr 2020
Copyright
© 2023 Lai Lai Soe. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DDA.2019.01.05
Author Info
Lai Lai Soe Yi Yi Htun Yee Yee Tin
Corresponding Author
Lai Lai SoeUniversity of Medicine, Magway, Myanmar
Figures & Tables


References
- Suman RK, Mohanty IR, Deshmukh YA (2014) The concept of drug utilization study. World J pharmacy and pharmaceutical sci 3: 352-362.
- WHO (2016a) Guidelines for ATC classification and DDD assignment, 19th ed., Oslo, Norway: WHO.
- Blix HS (2016) Measurement units of drug utilization. In: Elseviers M, Wettermark B, Almarsdóttir AB, Andersen M, Benko R et al. (eds.) Drug utilization research method and applications. 1st ed. UK: John Wiley & Sons, Ltd, 58-61.
- Campbell S, Wettermark B, Andersen M (2016) Defining and developing quality indicators for drug utilization. In: Elseviers M, Wettermark B, Almarsdóttir AB, Andersen M, Benko R et al. (eds.) Drug utilization research method and applications. 1st ed. UK: John Wiley & Sons, Ltd, 126-138.
- WHO (2016b) ATC/ DDD Index 2016 [online]. Oslo, Norway.
- Paudel KR, Sharma M, Das BP (2008) Prevalence of antimicrobial chemotherapy in hospitalized patients in the department of medicine in a tertiary care center. Nepal Med Coll J 10: 91-95. [Crossref]
- Wecker L, Crespo L, Dunaway G, Faingold C, Watts S (eds.) (2010) Principles of antimicrobial use. In: Brody’s human pharmacology molecular to clinical. 5th ed. Philadelphia: Mosby Elsevier 511-524.
- Cripps AW, Kyd J, Foxwell R (2004) Bacterial respiratory infections: the global burden of disease and strategies for control. Australian J med sci 25: 124-128.
- Aye-Thi-Khing (2013) Prescribing patterns of antimicrobials and culture and sensitivity patterns of microorganisms in medical wards of YGH. M. Med. Sc (Pharmacology). Thesis, University of Medicine 1, Yangon.
- Gumbo T (2011) General principle of antimicrobial therapy. In: Brunton LL, (ed.). Goodman & Gilman’s the Pharmacological Basis of Therapeutics, 12th ed. McGraw Hill. 1365-1377.
- Leekha S, Terrell CL, Edson RS (2011) General Principle of antimicrobial therapy. Mayo clin proc 86: 156-167. [Crossref]
- Han-Lin-Aung (2015) Drug utilization of Antibiotics in No (2) Defence Services General Hospital (1000 Bedded), Naypyitaw. M. Med. Sc (Pharmacology). Thesis, Defense Service Medical Academy, Yangon.
- Katakam P, Elfituri AA, Ramadan ZH, Abadi OG (2012) A retrospective study on antibiotic use in different clinical departments of a teaching hospital in Zawiya, Libya. Ibnosina J med biomed sci 4: 13-15.
- Bada MZ (2014) Antimicrobials utilization pattern in Governmental Hospital in Palestine measured using WHO ATC/DDD methodology. Master of clinical Pharmancy thesis, An-Najah National University Nalbus, Palestine.
- Khan FA, Singh VK, Sharma S, Singh P (2013) A prospective study on the antimicrobial usage in the medicine department of a tertiary care teaching hospital. J Clin Diagn Res 7: 1343-1346. [Crossref]
- Palappallil DS (2015) Pattern of use of antibiotics following snake bite in a tertiary care hospital. J Clin Diagn Res 9: 5-9. [Crossref]
