An Osteoplastic Advancement Flap, “Sandwich” Osteotomy and Application of a Skin Regeneration Template Prior to Implant Placement
A B S T R A C T
Introduction: Following oral cancer resection patients will have differing degrees of morbidity with regards to mastication, speech and aesthetics and this can be a difficult problem to manage. We present a case that describes an innovative technique involving implant placement and deepening of the labial sulcus in the atrophic mandible of a post-operative oral cancer patient to facilitate partial denture retention.
Methods: a 70-year-old female patient presented with significant vertical and horizontal bone atrophy and a shallow, tethered labial sulcus in the anterior mandible, following cancer resection of the floor of mouth and alveolar ridge. She was unable to retain a partial denture. An initial procedure included an osteoplastic advancement flap and a horizontal "sandwich" osteotomy as a combined approach that improved the bone volume from a Cawood & Howell classification grade V to grade II. A sulcoplasty and insertion of Integra@ skin regeneration system improved sulcus depth in a second procedure. Dental implants were successfully placed 4 months after bone augmentation to allow retention of a lower partial denture.
Results: These staged procedures were carried out with excellent healing and no complications in the post-operative 6 months.
Conclusion: This technique for gaining bony height and width, with improved sulcus depth in an atrophic mandible is a useful adjunct in the rehabilitation of post-operative oral cancer cases. Maintaining the periosteal attachment in the osteoplastic flap promotes excellent healing in patients who have received adjunctive radiotherapy treatment in this safe and effective osteotomy procedure.
Keywords
Oral rehabilitation, sandwich osteotomy, skin regeneration system
Introduction
Oral rehabilitation of post-operative cancer survivors can be a challenge particularly in cases when the resection has been extensive. The loss of hard and soft tissue, reconstruction with local or distant flaps and post-operative soft tissue scar contraction, can make the prescription and retention of oral prostheses difficult [1]. This has a profound effect on patients' quality of life [2]. Titanium implant placement can give invaluable retention for prosthetic rehabilitation with positive outcomes for patients and an improved quality of life [3]. Good implant success rates have been widely reported in those who have, or have not, received adjunctive radiotherapy [4]. We present a challenging case in which a combined approach of sandwich osteotomy, implant placement and soft tissue management with a skin regeneration template leading to successful oral rehabilitation of an oral cancer patient.
Case Report
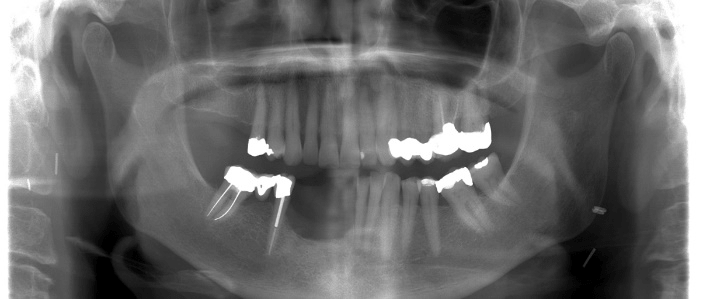
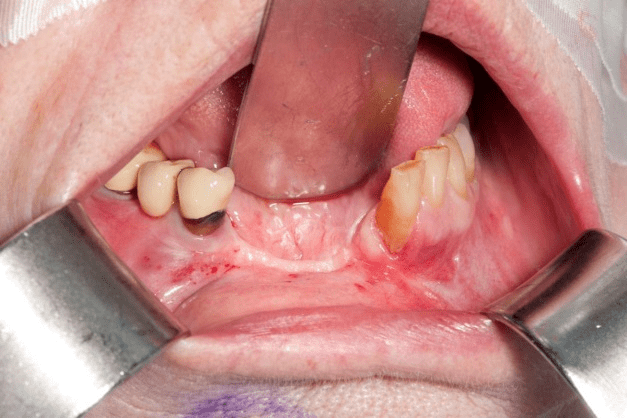
A 70-year-old female patient underwent surgical excision of an oral squamous cell carcinoma and selective neck dissection under the care of the Oral and Maxillofacial Surgery Department in a district general hospital. For surgical clearance she had the extraction of the lower right incisors, canine and first premolar teeth and an alveolectomy. 3 years following original surgery our laboratory technicians were unable to make her a satisfactory and retentive lower partial denture due to an atrophic alveolar ridge, and shallow labial sulcus (Figure 1.1, 1.2). A CT scan demonstrated this portion of the mandible as a Cawood & Howell classification grade V.
Figure 1.1: Orthopantomogram demonstrating atrophic alveolar ridge in the right anterior mandible.
Figure 1.2: very shallow and tethered labial sulcus.
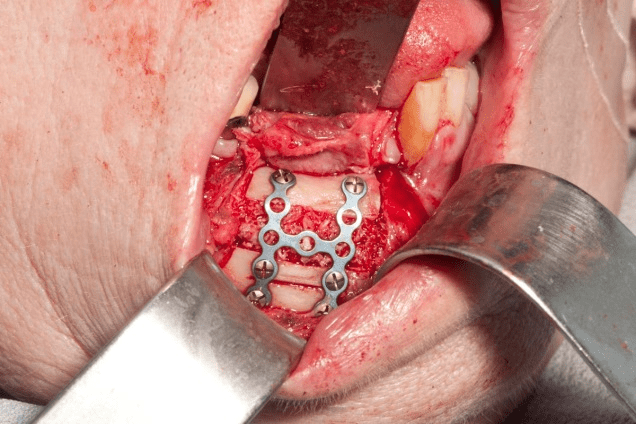
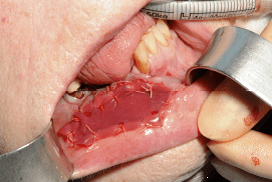
The patient underwent an initial procedure to heighten the alveolar ridge to accommodate implant placement at a later date. A gingival, 3-sided flap was raised, and a horizontal osteotomy performed, maintaining periosteal attachment of the attached gingivae to the bony segment. This was then lifted, and allogenic, cancellous bone packed into the created space. This was then plated into its new position and closed (Figure 1.3) to give a sandwich osteotomy.
Figure 1.3: sandwich osteotomy held in place with an H-shaped titanium plate.
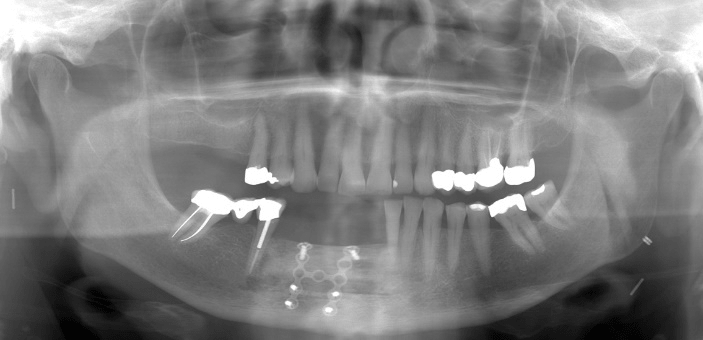
A new OPG radiograph showed improved height and integration (Figure 1.4) and a Cawood & Howell Grade II. The labial sulcus however had been scarred from original surgery and the sandwich osteotomy had caused further stretching and tethering.
Figure 1.4: Orthopantomogram showing improved bone height in the anterior mandible.
In a second procedure 4 months later the H-shaped plate was removed, and 2 titanium implants were placed and the labial sulcus was released. A two-layered skin regeneration system (Integra@, Integra Life Sciences Corp, Plainsboro, NJ, USA) was placed onto the exposed bone and in to the newly created lingual sulcus and sutured in to place to encourage regrowth of a functional dermal layer (Figure 1.5).
Figure 1.5: skin regeneration system sutured in place.
This was covered by a removable acrylic splint to encourage close contact of the system to bone. An acrylic block sat over the edentulous ridge and Adams' clasps aided retention on the lower right first premolar and lower left first molar. The top silicone layer of the regeneration system was removed 3 weeks later, and the region left to granulate over the top of the neodermal layer that had formed over bone.
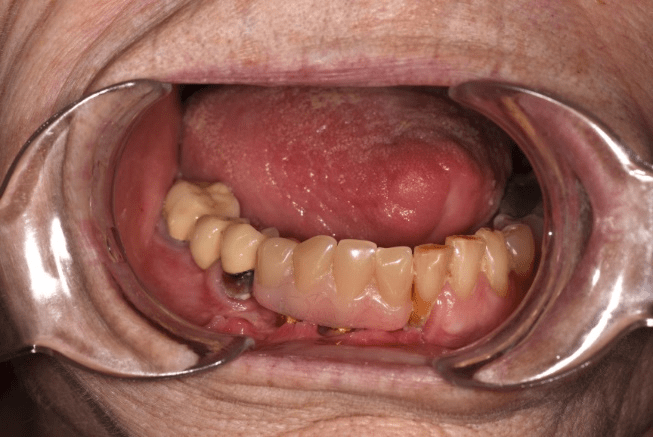
Six months following this course of treatment the patient has improved sulcal depth and soft tissue mobility. Importantly the patient was then able to have a retentive and comfortable lower implant retained partial denture constructed (Figure 1.6).
Figure 1.6: implant retained lower partial denture with good soft tissue movement.
Discussion
Dependent on location, size and aggression of the malignant lesion surgery for oral cancer often requires the removal of teeth and bone. The loss of these hard tissues and post-operative soft tissue scar contraction can make the prescription and retention of oral prostheses difficult [1]. Post-operative healing can be unpredictable with some patients having severe scar contraction and associated distortion of oral anatomy [5]. The sandwich osteotomy procedure has been previously described and is well accepted to improve bone height and width in the mandible to facilitate implant placement [6]. In cases of previous cancer resection, the mucosa and surrounding soft tissue is usually tethered. This can restrict its mobility and, although the tethering is released during the osteotomy to increase bone height and width, adequate closure would be inhibited causing a decrease in the depth of an already shallow labial sulcus.
The skin regeneration system encourages a neodermis to form on top of exposed bone in the presence of a blood supply from the peripheral mucosa. Success has been described working on a similar premise on exposed bone elsewhere in the head and neck region in one stage procedures [7]. We have had success using the Integra@ skin regeneration system intra-orally in a one stage procedure in the management of a mandibular defect in osteoradionecrosis following debridement of bone [8]. Once a neodermis has formed under the silicone layer of the 2 layered skin regeneration system after 3 weeks, granulation should be present, which leads to healing by secondary intention with minimal tissue contraction. The use of this system in the intra-oral environment aims to replicate the application of an artificial cellular dermis on defects of the head and neck, avoiding the need for further tissue transfer procedures that could cause additional donor site morbidity [9, 10].
Conclusion
This combined technique for gaining bony height and width in an atrophic mandible works well in post-operative oral cancer cases. The addition of deepening the labial sulcus also helps in the prescription of a partial denture and improves patient comfort and compliance. Maintaining periosteal attachment to the osteoplastic flap, with the addition of Integra@ skin regeneration system, promotes excellent healing in patients following cancer surgery alone and/or radiotherapy when combined with the sandwich osteotomy.
Funding
None.
Conflicts of interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 22, Aug 2019Accepted: Thu 19, Sep 2019
Published: Fri 27, Sep 2019
Copyright
© 2023 Andrea Beech. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ORD.2019.01.03
Author Info
Corresponding Author
Andrea BeechDepartment of Oral and Maxillofacial Surgery, Consultant Oral and Maxillofacial Surgery, Gloucestershire Royal Hospital, Gloucestershire Hospitals NHS Foundation Trust
Figures & Tables
References
- Finlay PM, Dawson F, Robertson AG, Soutar DS (1992) An evaluation of functional outcome after surgery and radiotherapy for intraoral cancer. Br J Oral Maxillofac Surg 30: 14-17. [Crossref]
- Roger SN, McNally D, Mahmood M, Chan MF, Humphris GM (1999) The psychological response of the edentulous patient following primary surgery for oral cancer: a cross-sectional study. J Prosthet Dent 82: 317-321. [Crossref]
- Chan MF, Hayter JP, Cawood JI, Howell RA (1997) Oral rehabilitation with implant-retained prostheses following ablative surgery and reconstruction with free flaps. Int J Oral Maxillofac Implants 12: 820-827. [Crossref]
- Weischer T, Mohr C (1999) Ten-year experience in oral implant rehabilitation of cancer patients: treatment concept and proposed criteria for success. Int J Oral Maxillofac Implants 14: 521-528. [Crossref]
- Rogers SN, Panasar J, Pritchard K, Lowe D, Howell R et al. (2005) Survey of oral rehabilitation in a series of 130 patients treated by primary resection for oral and oropharyngeal squamous cell carcinoma. Br J Oral Maxillofac Surg 43: 23-30DOI: . [Crossref]
- Laviv A, Jensen OT, Tarazi E, Casap N (2014) Alveolar Sandwich Osteotomy in Resorbed Alveolar Ridge for Dental Implants: A 4-Year Prospective Study. J Oral Maxillofac Surg 72: 292-303. [Crossref]
- Burd A, Wong PS (2010) One-stage Integra reconstruction in head and neck defects. J Plast Reconstr Aesthet Surg 63: 404-409. [Crossref]
- Beech A, Farrier J (2016) The use of Integra© skin regeneration system in an intra-oral mandibular defect in osteoradionecrosis. Int J Oral Maxillofac Surg 45: 1159-1161. [Crossref]
- Yura S, Ooi K, Izumiyama Y (2011) Repair of oral mucosal defects using artificial dermis: factors related to postoperative scar contracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112: 161-163. [Crossref]
- Girod DA, Sykes K, Jorgensen J, Tawfik O, Tsue T (2009) A cellular dermis compared to skin grafts in oral cavity reconstruction. Laryngoscope 119: 2141-2149. [Crossref]
