Airway Compromise Due to Extensive Subcutaneous Emphysema Following Trauma: A Case Report
A B S T R A C T
Subcutaneous or surgical emphysema (SE) following chest trauma is usually not of major concern in itself and tends to be self-limiting, provided the underlying cause has been addressed. Occasionally, a patient may present with massive SE which may threaten the patient’s airway and breathing. It is important for clinicians to have a management approach to such patients. Here we present such a case that was admitted to our hospital, describing the management approach and review the existing literature on the subject.
Keywords
Subcutaneous emphysema, surgical emphysema
Introduction
Subcutaneous (or surgical) emphysema (SE) is the presence of air in the subcutaneous tissues. Its presence implies communication between the pleural space and the subcutaneous space, for which the cause may be a penetrating injury or a fractured rib. Air escapes from the injured lung, causing a pneumothorax, and enters the subcutaneous space, causing subcutaneous emphysema. If air escapes freely from an open chest wound, surgical emphysema is much less likely to occur. If there be a driving force behind the air exiting the pleural space (e.g. tension pneumothorax) and there is nowhere to escape through the skin surface, massive SE ensues. This can extend from the patient’s head to lower limbs. The SE may be so extensive around the face, neck and chest regions that it compromises the patient’s airway and breathing.
Case Presentation
A 70-year-old male was brought to our emergency unit after being found unconscious outside his home four hours earlier. He had sustained blunt chest trauma from assault by community members throwing rocks at him. His comorbidities included chronic obstructive pulmonary disease (COPD) and previous pulmonary tuberculosis (PTB).
On examination, the patient had extensive SE from his head to feet. The skin around his thorax, neck and face was tense due to SE. His eyes were swollen shut due to significant periorbital subcutaneous swelling. He had severe respiratory distress and showed signs of airway compromise with tripod positioning, drooling, desaturation, stridor, and he was irritable and combative.
The source of SE was initially unclear as there was no obvious external injury to the patient, other than a small frontal head laceration. Examination of the patient proved challenging. Auscultation of the chest was difficult as significant SE gave the impression of decreased air entry bilaterally. On palpation of the patient’s back, a small flail segment of the right posterior lower ribs was noted, raising suspicion of right-sided pneumothorax. There were no clinical signs of tension pneumothorax, with trachea central normal blood pressure and no visible neck vein distension. X-ray imaging was available but would have meant a substantial delay in the patient’s care. Bedside ultrasound was unhelpful due to the extensive SE.
As the patient’s airway and breathing were both compromised, the treating team simultaneously prepared for a difficult intubation and thoracostomy tube insertion. The airway was assessed as Mallampati class 4, due to SE involving the tongue and pharynx. Preparations were made for surgical cricothyroidotomy, although this was also anticipated to be technically difficult due to the large amount of swelling around the neck with distortion of landmarks.
A thoracostomy tube was inserted on the patient’s right side with a small release of air noted. Thereafter, the patient’s condition slowly improved, and intubation was avoided. Within 30 minutes the patient’s SE had notably decreased and he no longer had stridor or drooling and was able to manage his secretions and speak. Within an hour he could sit up comfortably and within three hours he could open his eyes and give a brief history.
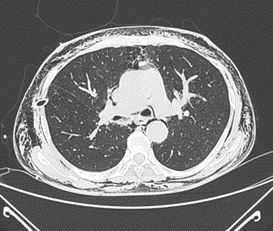
The patient was admitted to the Intensive Care Unit (ICU) for monitoring, where he was placed on non-invasive positive pressure ventilation for respiratory support. A chest X-ray was obtained which showed extensive SE, a small pneumomediastinum, bilateral expanded hyperinflated lungs, and the thoracostomy tube on the right (Figure 1). Computed tomography of the chest (Figure 2) showed significant SE, a small right pneumothorax, pneumomediastinum, fractures of ribs 8-10 on the right, and features of previous lung disease. The patient unfortunately deteriorated in ICU. Due to his background history of COPD and previous PTB, he developed progressive respiratory failure. He was subsequently intubated and ventilated but died the following day due to intractable hypoxia.
Figure 1: Chest X-ray. Extensive subcutaneous emphysema, lungs fully expanded and hyperinflated, thoracostomy tube on the right.
Figure 2: Computed tomography chest. Extensive surgical emphysema, thoracostomy tube on the right, pneumomediastinum. (Not seen on this image: fractures of right ribs 8-10, small right pneumothorax, features of previous lung disease).
Discussion
Subcutaneous emphysema (SE) is the infiltration of air or gas into the subcutaneous tissues. This is often a self-limiting and benign complication [1]. Surgical or subcutaneous emphysema is commonly encountered with blunt or penetrating trauma, surgical interventions, infections, ventilator-associated complications and even spontaneous aetiologies [1, 2].
The majority of cases are self-limiting, however in rare cases of extensive gas expansion, it may be life threatening. In these cases, massive SE may cause compartment syndrome, compress the trachea, prevent thoracic wall expansion and even compromise respiratory and cardiovascular drive [1, 2]. Massive SE following chest trauma compromising the airway has been rarely described in literature. In 2018, English literature documented a limited number of such cases, two of which were secondary to trauma [2]. Since then, only a handful of trauma related case studies have been described [3, 4].
The assessment and management of severe SE can be challenging. In the case of trauma, the presence of SE commonly suggests an underlying pneumothorax [5]. However, it may be difficult to identify which side of the thorax is affected, and cases have been described without a pneumothorax as the cause. Auscultating the lungs is difficult as the chest cavity is separated from the stethoscope by a layer of air and tissue. Ultrasound-guided diagnosis is equally difficult for the same reason. X-ray may contribute to diagnosis and decision-making, but may take too long if acute airway compromise is a concern. Interpreting the X-ray may be challenging, as a pneumothorax underlying significant SE can be difficult to diagnose [4, 6].
The described treatment options documented for this condition are varied in the literature. There are no guidelines on the management of SE, and there are only case-based recommendations. In severe cases with laryngeal oedema, tracheostomy has been performed in order to maintain an airway [7, 8]. However, this is very invasive and may prove technically very difficult to perform in a patient with severely distorted anatomy due to significant SE. In other instances, endotracheal intubation has been required in order to prevent complete airway collapse, in conjunction with bilateral thoracostomy tube placements [9]. Other treatments describe the insertion of bilateral subcutaneous drains or angiocatheters in order to treat SE as a time-buying initiative [3, 10-12]. Bilateral infraclavicular incisions extending into the subcutaneous tissues, also known as “infraclavicular blowholes”, have also been noted to decompress SE causing airway compromise [13, 14]. Although this has been described to be beneficial, it has also been noted to have negative effects as it may lead to localised infection and may result in cosmetic scarring [13, 14]. In our emergency unit, none of the abovementioned “other treatments” are promoted. The best described treatment option is single or bilateral tube thoracostomies, with or without suction [13-15].
Conclusion
Significant SE causing airway compromise is a rare complication in trauma cases. It may often be difficult to diagnose the source. In the case of trauma-related significant SE with airway compromise, target-directed tube thoracostomy is a rapid, effective, accessible and safe treatment option. If it is not clear as to which hemithorax is the source of SE, bilateral tube thoracostomies may be the safest option. Management of the airway (with intubation or provision of a surgical airway) is rarely necessary, but must be attended to without delay if indicated.
Conflicts of Interest
None.
Funding
None.
Ethics Approval
This case report was exempted from ethics review by the Biomedical Research Ethics Committee of the University of KwaZulu Natal, in keeping with the South African Department of Health Ethics Guidance (2014). All identifiers have been removed so that the case is anonymised and protected from deductive identification.
Article Info
Article Type
Case ReportPublication history
Received: Sat 11, Feb 2023Accepted: Fri 03, Mar 2023
Published: Wed 01, Nov 2023
Copyright
© 2023 George Oosthuizen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2023.01.01
Author Info
Hendry K Geraty S Čačala SR George Oosthuizen
Corresponding Author
George OosthuizenDepartment of Surgery, Ngwelezana hospital, University of KwaZulu Natal, Empangeni, South Africa
Figures & Tables

References
1. Kukuruza K, Aboeed
A (2022) Subcutaneous Emphysema. Treasure Island (FL): StatPearls Publishing. [Crossref]
2. Beard RG (2014)
Emphysema, Surgical. French's Index of Differential Diagnosis (Eleventh
Edition).
3. Olmstead D, Gelfand
G, Anderson I, Kortbeek JB (2018) A Case Report of Acute Airway Compromise due
to Subcutaneous Emphysema. Case Rep Med 2018: 3103061. [Crossref]
4. Tran Q, Mizumoto R,
Mehanna D (2018) Management of extensive surgical emphysema with subcutaneous
drain: A case report. Int J Surg Case Rep. 44: 126-130. [Crossref]
5. Harridine J, Sovani
M (2021) Spot the Pneumothorax. Cureus 13: e17177. [Crossref]
6. Melhorn J, Davies
HE (2021) The Management of Subcutaneous Emphysema in Pneumothorax: A
Literature Review. Curr Pulmonol Rep 10: 92-97.
7. Porhomayon J, Doerr
R (2011) Pneumothorax and subcutaneous emphysema secondary to blunt chest
injury. Int J Emerg Med 4: 10. [Crossref]
8. Pecora DV (1993)
Management of Massive subcutaneous emphysema. Chest 104: 655-656. [Crossref]
9. Harrison R, Knowles
S, Doherty C (2020) Surgical Emphysema in a Pediatric Tertiary Referral Center.
Pediatr Emerg Care 36: e21-e24. [Crossref]
10. Smith CT, Arshad W,
Dillenkofer M, Smith D (2020) Airway compromise from traumatic pneumothorax
with severe subcutaneous emphysema. BMJ Case Rep 13: e235843. [Crossref]
11. Sherif HM, Ott DA
(1999) The use of subcutaneous drains to manage subcutaneous emphysema. Tex
Heart Inst J 26: 129-131. [Crossref]
12. Robinson B (2018)
Rapid resolution of severe subcutaneous emphysema with simple percutaneous
angiocatheter decompression. J Surg Case Rep 2018: rjy173. [Crossref]
13. Herlan DB,
Landreneau RJ, Ferson PF (1992) Massive spontaneous subcutaneous emphysema.
Acute management with infraclavicular "blow holes". Chest 102:
503-505. [Crossref]
14. Johnson CHN, Lang SA, Bilal H, Rammohan KS (2014) In patients with extensive subcutaneous emphysema, which technique achieves maximal clinical resolution: infraclavicular incisions, subcutaneous drain insertion or suction on in situ chest drain? Interact Cardiovasc Thoracic Surg 18: 825-829. [Crossref]
15. Cerfolio RJ, Bryant AS, Maniscalco LM (2008) Management of subcutaneous emphysema after pulmonary resection. Ann. Thorac Surg 85: 1759-1763. [Crossref]
