Acute Aortic Occlusion with Acute Onset of Paraplegia and Severe Hyposthenia
A B S T R A C T
A 75-years-old man presented at our ED with acute onset of paraplegia and severe bilateral lower limb hyposthenia. The patient ‘s neurological assessment was negative except for lower limbs positive Mingazzini test. CT angiography detected a complete lack of opacification of the abdominal aorta immediately below the emergency of the inferior mesenteric artery, caused by a coarse thrombus in the left ventricle. We present a case of acute aortic and lumbar arteries thrombosis with paraplegia and no clear symptoms of acute limb ischemia, in which the motor deficit in the lower extremities was explained by anterior spinal cord syndrome secondary to acute occlusion of lumbar arteries.
Keywords
Arterial occlusive disease, thrombosis, aortic occlusion, acute paraplegia, hyposthenia
Background
Acute aortic occlusion (AAO) is a rare and infrequent medical condition with high mortality rate. Clinical symptoms depend on the level of the aortic occlusion and can be mistaken for stroke or similar neurological disease. It may appear under extremely various forms, from absolutely asymptomatic up to the most serious clinical presentations with severe pain and ischemia of the lower limbs, sometimes accompanied by paresthesia or paraplegia. Intravenous contrast enhanced Multidetector Computed Tomography (MDCT) is the imaging modality of choice for investigating aortic occlusion; MDCT also identifies possible comorbidities that can influence clinical management and therapeutic choices. We report a case of AOO with acute onset of paraplegia and severe hyposthenia.
Case Presentation
A 75-years-old man presented to our Emergency Department with acute onset of paraplegia and severe lower limbs hyposthenia. Acute symptoms arised,while he was seated, in a time lapse of one hour. The patient had a medical history of ischemic heart disease treated with PCI and stenting and controlled mild hypertension under drug medication, he had no history of previous trauma. Vital signs were normal except for PA of 140/80 mmHg. The cardiopulmonary examination was unremarkable, peripheral pulses were present but weak. The abdomen was slightly painful on palpation, skin was normal. Neurological assessment was negative except for positive Mingazzini test in the lower limbs.
Investigation
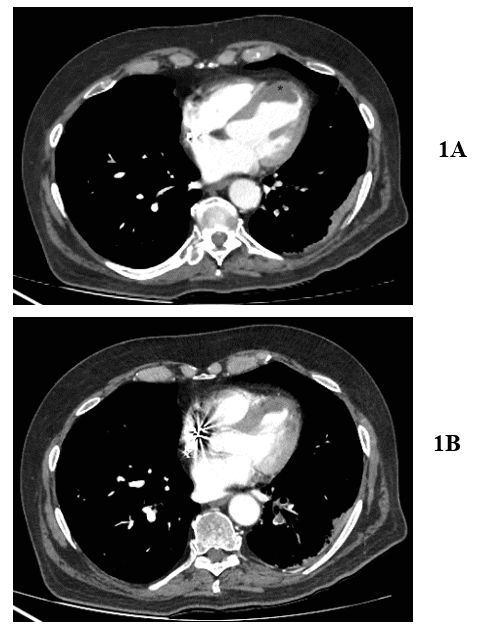
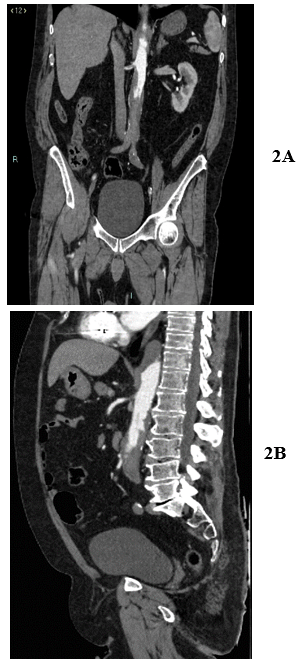
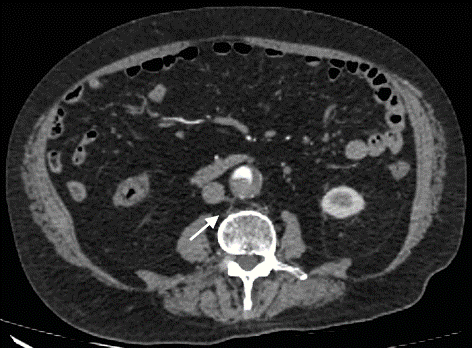
Laboratory tests showed a high white blood cell count (11x103/mm3), moderate high levels of C-reactive protein (2mg/dl) and urea (55 mg/dl). Coagulation tests and lactate were unremarkable. EKG was normal. Patient underwent MDCT angiography in emergency settings. Chest and abdomen CT angiography were performed (supine position, peripheral venous access of 18G in right antecubital vein with 120 ml of iodinated contrast material at a rate of 4 mL/sec). At MDCT examination, a defect of opacification adherent to the left ventricle wall was visualized, caused by an intracardiac thrombus (42x23 mm) and pulmonary embolism in the lower left lobe was detected (Figures 1A & 1B). Complete lack of intravenous opacification of the abdominal aorta was detected, which extended immediately below the emergency of inferior mesenteric artery (Figures 2A & 2B) to the iliac bifurcation with associated lack of opacification of lumbar arteries below the vertebral body of the first lumbar vertebra (Figure 3). Final diagnosis of acute abdominal aortic occlusion caused by cardiac embolus was achieved by CT, and the patient underwent embolectomy.
Figures 1: Axial CT images with iv contrast. A) thrombus (42x23 mm) displayed as a defect of opacification (*) adherent to left ventricle’s wall. B) pulmonary embolism in the lower left lobe.
Figures 2: CT images with iv contrast. A) coronal multiplanar reconstruction(MPR). B) sagittal MPR: lack of intravenous opacification of the abdominal aorta immediately below the emergency of inferior mesenteric artery, extended to the iliac bifurcation.
Figures 3: CT axial image with iv contrast. Lack of opacification of lumbar arteries below the vertebral body of the first lumbar vertebra (white arrow).
Discussion
AAO is a rare condition with high mortality rate, Grip et al. during a study of 20 years reported an incidence of 3.8 per 1 million person-years with mean age of 69.7 years [1]. AAO may be primary or secondary, primary aortic thrombosis occurs in an apparently normal aorta and the etiology of thrombus formation in a macroscopically normal aorta is not well understood, some causes are related to the patient's medical history: cancer chemotherapy, cocaine intake, essential thrombocythemia and some hypercoagulable states [2-4].
In case of secondary AAO, the most frequent etiologies are thrombosis in situ of an atherosclerotic aorta, an embolus in the aortic bifurcation, or thrombosis of an abdominal aortic aneurism; aortic thrombosis after a blunt trauma has also been described in a child [5-7]. In all cases, except for embolism, the pathogenesis is related to hypercoagulation disorder, hypotension or other low flow state or any other mechanism that affects platelet function, also high levels of stress-related hormones are considered a predisposing factor [8, 9]. Most patient present with bilateral acute limb ischemia with pain, coolness, paresthesia, absent pulses and mottling of the skin [10, 11]. Additional symptoms depend on level of thrombosis: acute renal failure in renal artery thrombosis, mesenteric ischemia in superior mesenteric thrombosis, gastric e\o hepatic failure in case of celiac trunk thrombosis. Johnson’s et al. described 10 out of 17 patients with AOO presented with acute onset of lower limbs paraplegia [11].
The motor deficit in the lower extremities can be explained partially by acute occlusion of the lumbar arteries with secondary anterior spinal cord syndrome and to lower limb muscles ischemia [12]. In case of AAO rapid diagnosis is essential, because ischemic skeletal muscles injuries often occur within 2 hours of ischemia.; in patients presenting with paralysis definitive limb loss can occur within 6 to 8 hours [13].In our patient the atypical clinical presentation with acute paraplegia and severe hyposthenia, was determined by the fact that external iliac arteries still showed minimal opacification and by the rapid onset of symptoms just one hour before the patient access to ED. According to previous published studies CT represents the imaging of choice in the diagnosis of AAO [14, 15]. Aortic occlusion was clearly demonstrated, and the contemporary thrombosis of lumbar arteries was clearly detected. Acute neurological symptoms require a rapid differential diagnosis with acute neurological syndromes in particular with spinal cord compression, therefore a careful neurological examination is important.
Although the CT diagnosis of acute aortic occlusion is not difficult, it is important to differentiate a thrombosed aorta from a saddle embolus: the therapeutic intervention in the former case is embolectomy, whereas a thrombosed aorta requires revascularization. Although in our case abdominal the aorta was apparently normal with no evidence of atherosclerotic disease, the diagnosis of primary AAO was excluded because of the evidence of a coarse thrombus in the left ventricle.
In conclusion acute aortic occlusion is a rare but life-threatening condition; lower limb ischemia is the most common clinical presentation, but a different presentation is possible depending on level of thrombosis. between these there is sudden paraplegia. MDCT angiography should be performed without delay for diagnosis, to distinguish primary from secondary AAO and to identify which branches of the aorta are affected.
Article Info
Article Type
Case ReportPublication history
Received: Wed 29, Apr 2020Accepted: Wed 13, May 2020
Published: Fri 15, May 2020
Copyright
© 2023 Stefania Tamburrini. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2020.02.03
Author Info
Daniela Viola Fabio Spinetti Giuseppe Mercogliano Giuseppe Sarti Ines Marano MariaVittoria Guerra Marina Lugarà Stefania Tamburrini Valeria Fiorini
Corresponding Author
Stefania TamburriniDepartment of Radiology, Ospedale del Mare, ASL NA1 Centro, Naples, Italy
Figures & Tables
References
- Webb KH, Jacocks MA (1988) Acute aortic occlusion. Am J Surg 155: 405-407. [Crossref]
- Verbeeck N, Cavez N, Plawny L, Weber J, Lens V (2014) Primary aortic thrombosis: role of enhanced multislice CT demonstrated in three exceptional cases. JBR–BTR 97: 76-80. [Crossref]
- Paulin Vera CM, Mateos Colin A, Calvo Arrojo G, Colodro García JM (2013) Acute aortoiliac thrombosis due to cocaïne intake. Ann Vasc Surg 27: 239.e1-239.e 4. [Crossref]
- Sincos IR, da Silva ES, Ragazzo L, Belczak S, Nascimento LD et al. (2009) Chronic thrombosed abdominal aortic aneurysms: a report on three consecutive cases and literature review. Clinics (Sao Paulo) 64: 1227-1230. [Crossref]
- Kaschwich M, Behrendt CA, Tsilimparia N, Kolbel T, Wipper SH et al. (2017) Management of acute aortic thrombosis. J Cardiovasc Surg (Torino) 58: 313-320. [Crossref]
- Vasdekis SN, Mastoraki S, Lazaris A, Moulakakis KG (2018) An Unusual Case of Acute Thrombosis of Abdominal Aortic Aneurysm without Acute Limb Ischemia. Aorta (Stamford) 6: 31-33. [Crossref]
- Kory LA (2000) Thrombosis of the abdominal aorta in a child after blunt trauma. AJR Am J Roentgenol 175: 553-554. [Crossref]
- Fernandes DD, Louzada ML, Sousa CA, Matzinger F (2011) Acute aortic thrombosis in patients receiving cisplatin- based chemotherapy. Curr Oncol 18: e97-e100. [Crossref]
- Pozzi AO, Bernardo E, Coronado MT, Punchard MA, González P et al. (2009) Acute arterial thrombosis in the absence of inflammation: the stress-related antiinflammatory hormone ACTH participates in platelet-mediated thrombosis. Atherosclerosis 204: 79-84. [Crossref]
- Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L et al. (1991) Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg 13: 452-458. [Crossref]
- El Kayali A, Al Salman MM (2001) Unusual presentation of acute bilateral lower limb ischemia (thrombosis of abnormal aortic aneurysm). Ann Saudi Med 21: 342-343. [Crossref]
- Watson TJ, Childers WK, Haga L, Calaitges J (2017) Acute Bilateral Lower Extremity Paralysis Secondary to Acute Thrombosis of an Infrarenal Abdominal Aortic Aneurysm. Aorta (Stamford) 5: 91-95. [Crossref]
- Blaisdell FW, Steele M, Allen RE (1978) Management of acute lower extremity arterial ischemia due to embolism and thrombosis. Surgery 84: 822-834. [Crossref]
- Bhalla S, Menias CO, Heiken JP (2003) CT of acute abdominal aortic disorders. Radiol Clin North Am 41: 1153-1169. [Crossref]
- Bertucci B, Rotundo A, Perri G, Sessa E, Tamburrini O (1997) Acute thrombotic occlusion of the infrarenal abdominal aorta. Its diagnosis with spiral computed tomography in a case. Radiol Med 94: 541-543. [Crossref]
