Acrometastasis as the First Presentation of Renal Cell Carcinoma
A B S T R A C T
Acrometastasis is the term used to describe secondaries present distal to the knee or elbow [1-3]. The occurrence of this is extremely rare. This accounts for 0.1% of all secondaries to the bone [1-5]. The presence of acrometastasis is considered to be a sinistrous sign and correlates with the advanced stage of the disease condition [1, 2, 5]. The majority of acrometastasis is from lung and gastrointestinal malignancies [1-3]. We present a case of a gentleman in his early 60’s, who presented with acrometastasis as the first sign of renal cell carcinoma.
Keywords
Finger swelling, acrometastasis, renal cell carcinoma
Background
Acrometastasis is a rare condition and accounts for only 0.1% of all secondaries. Most of this is from lung and gastrointestinal malignancies [1-3]. We had this gentleman who presented with non-traumatic swelling of the finger. The initial impression was it could be a soft tissue injury, rheumatological condition, inflammatory condition, or infection. Further workup revealed that this was acrometastasis from a renal cell carcinoma (RCC) which was not diagnosed before.
Case Presentation
A gentleman in his early 60’s presented to our Emergency Department with wrist pain and swelling in his left ring finger. He had pain in his left wrist for several weeks. The pain was mainly around the radial styloid. About 6 weeks back to his presentation, he reached over to unplug his computer (PC) and felt something go on his wrist, and he felt pain. This pain got aggravated after shoveling one week later. He took regular Naproxen and Paracetamol, but his wrist pain was not improving. This was worse on movement, especially on pronation and supination, and the pain was radiating to his elbow.
In addition to this, six weeks ago, he was lifting a log and felt a sharp pain in his left ring finger. The pain settled down, but days later the finger started to become swollen. He was seen by his GP (General Practitioner) and the GP clinically ruled out gout, and he was given painkillers. He did not have any background medical history, he was not on any medication and he was not allergic to any drugs. He works as a civil engineer, and he does an office-based job. He is a non-smoker and rarely drinks alcohol.
On examination in our department, his left ring finger was quite swollen, especially at the middle phalanx. But there was no redness or tenderness. He was able to flex his finger, however, his range of movement was restricted due to the swelling. Concerning his wrist, there was no swelling, redness, or bruising. There was significant tenderness on the distal radial styloid. His pronation and supination were limited due to the pain. The initial impression at that time was a diagnosis between a soft tissue injury, a repetitive strain injury, inflammation, rheumatic conditions, or osteomyelitis.
I Initial Investigations
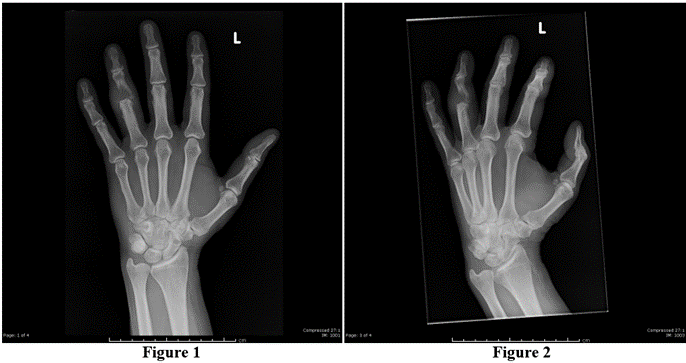
Basic blood tests including uric acid and inflammatory markers were carried out. Results of these were unremarkable except for slightly raised ALT at 51. X-ray of the wrist and hand showed a destructive lytic lesion at the base of the middle phalanx of the ring finger, with associated soft tissue swelling. The bone cortex was destroyed, indicating an aggressive type of lesion.
Figures 1 & 2: A plain radio-graph of the hand showing destructive lytic lesion involving proximal half of the middle phalanx of the ring finger of the left hand, with surrounding soft tissue swelling.
II Differential Diagnosis
Based on the X-ray findings, a primary or secondary bone tumor was considered. Osteomyelitis of the finger was also thought about.
III Further Investigation and Management
He was referred to the orthopedic team, and the plan was to do a MRI (Magnetic Resonance Imaging) of the hand and finger. Since the patient suffers from extreme claustrophobia, initially ultrasound of the finger was carried out. The ultrasound showed features of a solid vascular tumor within the medulla of the middle phalanx with breach in cortex. It was involving the proximal interphalangeal joint. When MRI was done at a later stage, it showed bone destruction with the tumor spreading into the soft tissue, with significant swelling of the ring finger.
When he was reviewed in the orthopaedic clinic, he was also complaining of pain around the elbow, hence an x-ray of the elbow was performed, which showed another lytic lesion in the radial head. The plan made at that point was to refer him to the Bone Tumor Unit at a Specialty Hospital and also to do a CT scan of the chest, abdomen, and pelvis, (CT CAP) to look for other lesions.
A CT CAP and the whole-body bone scan were done the next day. This showed an 8.5cm tumor in the left kidney. The bone scan showed skeletal metastasis of the left radial head, middle phalanx of the left ring finger, and posterior left ninth rib. It was concluded that the patient has a left renal primary tumor with lytic secondaries in the bone. He was referred to Urology Multi-Disciplinary Team (MDT) for management of his renal tumor. A week later, he was admitted electively into the hospital and an Ultrasound guided biopsy was taken from the finger.
Figure 3: Coronal magnetic resonance image showing metastatic growth spreading into the soft tissue and significant swelling over the middle phalanx of the ring finger.
The result of this was consistent with grade 1-2 clear cell renal carcinoma, showing focal necrosis. A staging CT head was also carried out which turned out to be normal.
IV Treatment
During the MDT meeting, consideration was given to cytoreductive nephrectomy, however, it was decided it may be beneficial to receive immunotherapy first. He was commenced on Ipilimumab, Nivolumab, and Zoledronic acid. It is possible that ongoing COVID pandemic also might have played a part in the decision making. After commencing immunotherapy he had febrile symptoms and he was admitted to the hospital and treated for sepsis.
After 2 months, the therapy had to be held due to grade 3 immunotherapy-related rash and grade 3 hepatitis which were treated successfully with steroids. After approximately three months, Nivolumab was reintroduced, which resulted in further hepatitis. Hence further immunotherapy was discontinued. MDT advice was to continue on a 'watch and wait' approach with interval scans in three months.
V Outcome and Follow Up
A CT CAP done after 7 months of diagnosis showed that the primary tumor has responded to the treatment. The Oncologist raised a concern about finger lesion getting worse and not responding to radiotherapy (RT). A further bone scan was done eight months after the presentation and it showed a new lesion in the left distal femur. Hence, he was referred to and was seen in the Bone Tumor Unit. Amputation of his finger was carried out. A further CT CAP done 11months after the diagnosis demonstrated enlarged sub pleural lymph node in the left lung. Patient was started on palliative Chemotherapy with Cabozatinib and palliative radiotherapy for the skeletal lesions. A new scan done 15 months after the diagnosis, showed reduction in the size of the renal mass and the lung nodule. Currently the patient is 18 months post diagnosis. He had 7 cycles of Chemotherapy and also had local radiotherapy for his skeletal lesions.
VI Timeline of Events
0 Day - Presentation with painful wrist and swollen finger. X-ray showed a lytic lesion on the ring finger.
9 Days - Ultrasound showed solid vascular tumor in the medulla of middle phalanx.
11 Days - Orthopaedic clinic review, X-Ray Elbow showing lytic lesion on the radial head.
12 Days - CT CAP and Bone scan, Showed Primary renal tumor and multiple bone secondaries.
01 Month - US-guided biopsy - Grade 1-2 Clear cell RCC.
1.5 Months - Immunotherapy commenced.
2.5 Months - Immune-related hepatitis, Immunotherapy stopped.
5.5 Months - Re-challenging treatment stopped due to further hepatitis.
7 Months - CT CAP showing - Primary tumor responding to treatment.
8 Months - Bone scan showing new secondary on the femur.
10 Months - Amputation of the left-hand ring finger.
11 Months - Enlarged sub pleural lymph node in the lung.
12 Months - Palliative Chemotherapy with Cabozatinib.
13 Months - Palliative Radiotherapy to the skeleton.
15 Months - Reduction in size of renal mass and lung nodule.
18 Months - Current status --Receiving Chemotherapy and palliative Radiotherapy.
Discussion
Acrometastasis is a term used to describe secondaries present distal to the knee or elbow [1-3]. This accounts for 0.1% of all secondaries to the bone [1-5]. In the majority of cases, acrometastasis is spotted in patients who are formally diagnosed to have cancer [1, 2]. The median time from diagnosis of the primary tumor to development of acrometastasis was found to be 24 months (range 0.7 - 156) [2]. 10% of patients who seek consultation, have not been diagnosed to have cancer [1, 2]. The mean age of acrometastasis was found to be 59 and the median age was 62 [3, 6]. Men were found to be more affected in comparison to women, mainly because of the fact the most commonly associated primary tumor which is lung cancer is more predominant in men [1-3, 5, 6].
The presence of acrometastasis is considered to be sinistrous sign, which correlates to the finding that it is encountered in patients with later stages of the oncological disease and carries a poor prognosis [1, 2, 5]. The mean survival was found to be around six months, after the diagnosis of acrometastasis [1-3, 5, 6]. It was interesting to find that patients with urological cancer who presented with acrometastasis survived longer than patients who had other primary cancer [1, 3]. In addition, it was also noted that patient characteristics like age, sex, location, and type of metastasis did not alter survival statistics [3].
There has not been any association documented between right and left hands, although some have reported greater incidence in the dominant hand due to more frequent trauma. [1, 5]. Approximately 7% to 10% of patients had encountered lesions in both hands [3, 5]. Acrometastasis are more commonly seen in the distal phalanges of fingers. and the thumb was the most common digit involved [1, 3, 5, 6]. It is presumed to be due to reduced circulatory speed which promotes secondary tumor growth [7, 8].
The specific mechanism of transmission of tumor cells to the hand is still ambiguous. An increased vascularity and trauma have been offered as a potential explanation [2, 5, 6]. Any kind of trauma can lead to the release of prostaglandins and other chemotactic factors that can enhance the cell migration and adhesion in these anatomical regions [9, 10]. Literary scrutiny revealed that acrometastasis are frequently associated with Pulmonary cancer (about 36-40%), Gastrointestinal cancer (about 19-20%), and Genitourinary tract neoplasm (10-13%) [3, 6]. Other primary tumors which can lead to acrometastasis can be found in the neck, breast, pelvic, skin, bone, and blood [3].
Acrometastasis can present as swollen, erythematous, painful lesions over the soft tissue and bone. This mimics benign conditions resulting in clinical misdiagnosis. Due to common signs and symptoms, acrometastasis needs to be differentiated from other conditions like inflammatory lesion, osteomyelitis, whitlow, cyst, pyogenic arthritis, gout, rheumatoid arthritis, tuberculosis, tenosynovitis, ganglion, etc [1, 2, 5].
Renal Cell Carcinoma (RCC) has a high incidence of bone metastasis. It is estimated that about one-third of patients with advanced RCC endure bone metastasis [11]. However, acrometastasis is uncommon and represents only 0.1% of the bone metastasis. Renal cell carcinoma is responsible for only 10-12 % of these uncommon lesions. [5, 12]. The clinician must maintain a high index of suspicion while assessing patients with RCC who present with swelling of fingers.
There is a lack of established guidelines for the treatment of acrometastasis [1, 2, 11]. The main goal of treatment is pain relief and preservation of hand function in the setting of surgery [1, 2, 6]. This is achieved alongside with treatment of primary tumors. Even though amputation remains the mainstay treatment option, other treatment options that are available with scientific advancements, which include radiotherapy, chemotherapy, immunotherapy, and combination treatments [1, 3, 5, 6, 11].
What was Different in our Patient?
Our patient was a healthy male with no previous medical co-morbidities. He was not on any regular medications. He falls approximately into 10% of patients who have no formal diagnosis of cancer at the time of seeking medical assistance which led to his diagnosis. Most acrometastasis occurs with lung and gastrointestinal malignancies. Our patient had Renal Cell Carcinoma. Even though one-third of patients with RCC get bone metastasis, the share of acrometastasis is approximately 0.01%. Literature review suggests the distal phalanx is the commonest area for Acrometastasis. But our patient had it in the middle phalanx.
Learning Points
1. Acrometastasis from malignancies are rare and this is more so with RCC.
2. Acrometastasis though rare, it exists and can present as limb pathology.
3. Among the patients who present with finger swelling, this needs to be considered as a differential along with other benign conditions, especially if they have a background diagnosis of malignancy.
Logistic Support
Janet Bird, Jane Thomas, Emergency Department secretaries, WGH.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 16, Jan 2023Accepted: Tue 31, Jan 2023
Published: Mon 13, Feb 2023
Copyright
© 2023 Deepak Verma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2023.01.01
Author Info
Deepak Verma Antony Mathew Rose-Anne Nunoo Mekha Maria John Mudit Jain Syeda Nabila Ali
Corresponding Author
Deepak VermaWithybush General Hospital Haverordwest, Wales, UK
Figures & Tables

References
1.
Mavrogenis AF, Mimidis G, Kokkalis ZT, Karampi ES, Karampela
I et al. (2014) Acrometastases. Eur J Orthop Surg Traumatol 24: 279-283.
[Crossref]
2.
Umana GE, Scalia G, Palmisciano P,
Passanisi M, Da Ros V et al. (2021) Acrometastases to the Hand: A Systematic
Review. Medicina (Kaunas) 57: 950. [Crossref]
3.
Cattelan M,
Dumontier C (2021) Metastatic tumor
of the hand - Three new cases and a literature review. J Plast Reconstr
Aesthet Surg 74: 2163-2168. [Crossref]
4.
Kerin R (1983) Metastatic tumors of the hand. A review of the
literature. J Bone Joint Surg Am 65: 1331-1335. [Crossref]
5.
Flynn CJ, Danjoux C, Wong J, Christakis M, Rubenstein J et
al. (2008) Two cases of acrometastasis to the hands and review of the
literature. Curr Oncol 15: 51-58. [Crossref]
6.
Afshar A, Farhadnia P, Khalkhali H (2014) Metastases to the
hand and wrist: an analysis of 221 cases. J Hand Surg Am 39: 923-932. [Crossref]
7.
Asencio
G, Hafdi C, Pujol H, Allieu Y (1982) Osseous metastases in the hand. A general review of three cases. Ann Chir
Main 1: 137-145. [Crossref]
8.
Viswanathan
PN, Rangad F, Roul RK (1996) Metastases to the Hand from Carcinoma of the Lower
Alveolus. J Hand Surg Am 21: 544-546. [Crossref]
9.
Sipahioglu
S, Zehir S, Ozkanli, U (2012) Nasopharyngeal carcinoma with hand metastasis. J
Hand Surg Eur Vol 37: 578-579. [Crossref]
10. Tolo
ET, Cooney WP, Wenger DE (2002) Renal cell carcinoma with metastases to the triquetrum: case report. J Hand Surg Am 27: 876-881. [Crossref]
11. Chen SC, Kuo PL (2016) Bone Metastasis from Renal Cell Carcinoma. Int J Mol Sci 17: 987. [Crossref]
12. Ghert MA, Harrelson JM, Scully SP (2001) Solitary renal cell carcinoma metastasis to the hand: the need for wide excision or amputation. J Hand Surg 26: 156-160. [Crossref]
