A Systematic Review of the Literature for the Effects of Music on Dementia Patients
A B S T R A C T
Introduction: There are over 100 different forms of dementia which is a broad term employed to describe symptoms effecting the brain caused by neurological and vascular diseases. It is a neurological disease that results in a decline in cognitive, social and physical disability which currently has no cure. The prevalence is expected to triple by 2050, due to the aging population trends in Canada. It has been estimated that 24.3 million people have dementia, and there are 4.6 million new cases annually, which accounts for one case every 3 seconds globally.
Objectives: This systematic review examines the effects of music therapy on behavioral psychological symptoms of dementia and the quality of life.
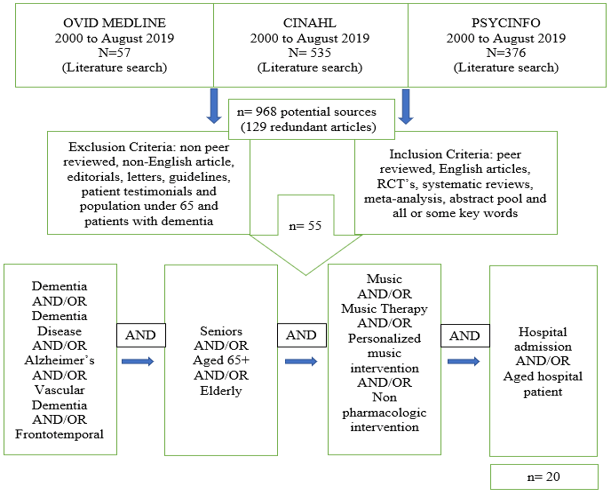
Methods: A systematic literature search was performed in Ovid Medline, CINAHL and PsycINFO from January 2000 until August 2019. A data abstraction template was employed to for data management and organization. We included all peer reviewed, English articles, RCT’s, systematic reviews, meta-analysis, abstract pool and all or some key words.
Results: From 968 potentially relevant records, 55 studies were evaluated for eligibility, and 20 met the inclusion criteria. Overall the studies showed a significant impact on mitigating agitation, reducing BPSD and improving memory, cognition, QOL and decreasing anxiety and symptoms associated with depression.
Conclusion: The role of musical interventions found in the literature demonstrates the benefits of music therapy on dementia patients due to its positive effects on BPSD, quality of life and other behavioral symptoms.
Keywords
Systematic review, music therapy, dementia, BPSD, quality of life, nonpharmacological intervention
Background and Significance
Dementia is a broad term that describes the symptoms affecting the brain caused by neurological and vascular diseases. It is a progressive and neurodegenerative disorder of the brain leading to brain cell death and tissue loss. Symptoms of dementia include memory loss, minimal thinking, loss of language, loss of independence, confusion, agitated behavior, inability and loss of interest to perform everyday activities, and problem-solving skills [1]. A chronic condition, dementia, can interfere with daily living such as bathing, eating, dressing and toileting independently. Some common forms of dementia are Alzheimer’s disease, Lewy Body Dementia, Vascular Dementia and Frontotemporal Dementia, which may vary in symptomatology [1].
Some forms of dementia have a strong genetic component and one of the causes include advancing age. Other risk factors include lower level of education, hypertension, obesity, smoking after the age of 65, diabetes, depression, physical inactivity, and social isolation [2]. The treatment depends on its underlying cause and targets symptom reduction and improved quality of life as there is no cure for dementia. Dementia is more common amongst women than men [3]. Some potential preventative strategies include regular exercise, avoidance of smoking/alcohol, healthy diet, maintaining a healthy blood pressure and cholesterol [4].
Table 1: Definitions of Key Terms.
|
Key Terms |
Definitions |
Reference |
|
Dementia |
Dementia is defined as the deterioration in memory, behavior, cognitive thinking and the inability to conduct everyday basic activities. It is a chronic progressive neurological disorder. Dementia is associated with emotional and behavioral problems which also decrease the quality of life. |
WHO, (2019) [4] |
|
Alzheimer’s Disease (AD) |
AD is the most common form of dementia that causes problem with the memory function, cognitive thinking, and behavior. Symptoms progress overtime and get severe enough to affect the daily tasks and function. |
Alzheimer’s Association, (2019) [22] |
|
Vascular dementia (VD) |
VD is the second most common form of dementia. It is described as a set of symptoms that include issues with problem solving/language, memory loss and cognitive issues. This is caused by brain damage which develops after a stroke and blocks the arteries in the brain blocking the blood flow. When blood flow is impaired, it is possible for the blood vessels to be damaged with reduced circulation. |
Mayo Clinic, (2019) [48] |
|
Lewy Bodies (LB) |
LB is a form of dementia which is associated with a protein called alpha-synuclein. This is an abnormal deposit that affects the chemicals in the brain and leads to problems with movement, mood, behavior and thinking. |
NIH, (2019) [49] |
|
Frontotemporal Dementia (FD) |
FD is a group of disorders which is a form of dementia. It causes progressive nerve cell loss in the frontal lobe or temporal lobe of the brain. This leads to a deterioration in behavior, personality issues and difficulty in comprehending language. |
Alzheimer’s Association, 2019 [22] |
|
Music |
Music is an art and expression of emotions. “It is the art of ordering or sounds in succession, in combination, and in temporal relationships to produce a composition having unity and continuity” |
Merriam-Webster, 2019 [45] |
|
Music Intervention (MI) |
MI is defined as a therapeutic setting where music is controlled to accomplish a psychological, physiological and emotional well-being during a treatment of a disease. |
Pedersen et al. (2017) [46] |
|
Music Therapy (MT) |
MT is a music intervention that is used to accomplish therapeutic goals of individuals by a professional who has completed a music therapy program. It addresses physical, cognitive, emotional and social needs. Music therapy helps people express themselves when avenues of communication are difficult. |
American Music Therapy Association [AMTA], (2019) [47] |
|
Personalized Music Intervention (PMI) |
PMI is a non-pharmaceutical approach which utilizes music to help treat patients who have a clinical condition and disorder. Some symptoms include depression, anxiety, agitation and dementia. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
|
Behavioral and Psychological Symptoms of Dementia (BPSD) |
BPSD, also known as neuropsychiatric symptoms, represents a group of cognitive symptoms and behavior occurring in patients with dementia. BPSD is common in dementia irrespective of the subtype. BPSD includes, hallucinations, agitation, violent motor behavior, anxiety and irritability. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
|
Pharmacological Intervention (PI) |
PI is the use of a variety of medication to treat BPSD and other effects of dementia such as the symptom’s and side effects. The medications include antidepressants, AChEI, mood stabilizers, typical and atypical antipsychotics, benzodiazepines, memantine and other drugs. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13]
|
|
Nonpharmacological Intervention (NI) |
NI is the use of therapies excluding medications to improve the quality of life for patients with dementia. The therapy interventions are classified into various different categories. This includes cognitive/emotion-oriented intervention such as stimulated presence therapy, reminiscence therapy and validation therapy. Sensory stimulation includes light therapy, music therapy, aromatherapy and acupuncture. Behavior management technique and psychological intervention such as exercise and animal-assisted therapy. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
Dementia Strategy for Canada
A dementia strategy was implemented on June 22, 2017 which was passed as Bill C- 233 known as the National Strategy for Alzheimer’s Disease and Other Dementias Act [5]. The objective of the national strategy is to prevent dementia, advance therapies, find a cure, and lastly improve the quality of life for people with dementia (PWD) and their caregivers [2]. The prevention of dementia will require advances in research. The promotion of effective interventions is key, expanding awareness of the modifiable risk factors for public knowledge and supporting measures that contribute to social environments to healthy living. The advance therapies/cure objective is to review strategic dementia research, develop therapeutic approaches, engage PWD and caregivers in various forms of therapies. Improvement in the quality of life for PWD and caregivers has a goal to promote early diagnosis, accession to care from beginning to end of life, and improve support for caregivers through resources. There are 6 key themes in the development of this strategy, which is support for caregivers and PWD, access to dementia services, awareness, coordinated care and trained professionals for dementia [6].
The dementia strategy includes a commitment to raise awareness across Canada to help reduce stigma. Healthy living reduces the onset of dementia, and it is recommended to maintain a healthy lifestyle to prevent it. The dementia strategy of Canada possesses a vision to achieve a good quality of life for PWD, to make life long/easy, and make caregivers the centre of this strategy [2]. There are 5 principles that guide action based on dementia. The 5 principles are prioritizing the quality of life by living well and long, having access to quality care and a supportive community. The second principle is respect and value diversity including people most at risk, inclusivity which includes diversity of all forms, distinguishing indigenous needs and keeping the community involved [2].
The third principle is respect for human rights for those living with dementia, enable them to participate and make their own decisions. The perspective of caregivers is also taken into consideration since they are the ones caring for PWD. The fourth principle is evidence informed. Evidence informed decision requires to retrieve research findings and data to make evidence informed decisions. All forms of knowledge are taken into consideration when gathering evidence as it is essential to work together in order to build evidence. The last principle is result focused which has a measurement indicator to track progress, accountability of reporting the gathered results to parliament, and a flexibility to evolve [2].
Pillars for Dementia Strategy in Canada
There are 5 pillars in Canada that are important for the implementation of a National Pan-Canadian strategy which is collaboration, research/innovation, surveillance/data, information resources and skilled workforce [2]. Collaboration is building on partnership and collaborating on dementia diseases which include people living with dementia and caregivers. Care providers, community organizations, social services and research groups all have a role to play in order to achieve the national objective, which is to prevent dementia, advance therapies, find a cure and improve the quality of life for PWD. Research and innovation are significant in the implementation of the dementia strategy. This helps to test out new approaches to therapies and improving the quality of life. Canada is committed to supporting research that will find a cure and promote the effective practices across the country [2].
Surveillance and data provide good information on the impact of dementia in Canada. Surveillance helps to detect the type of population most affected and more at risk. It will also identify the type of activities needed to support the strategy [2]. Skilled workforce in Canada is diverse which includes researchers, health professionals, caregivers and other care providers. A sufficient workforce helps to improve the care of dementia patients. Canada will need more care providers since the population of dementia is expected to increase. Institutions will need programs offering dementia training and care to ensure the workforce is knowledgeable about dementia. It is crucial for the workforce to be informed about the knowledge and skills to improve the quality of care [2]. There are many non-pharmacological interventions that help people with dementia. Interventions include massage, aromatherapy, music therapy, animal assisted therapy and multisensory stimulation. Music therapy was the most effective therapy because PWD who had trouble speaking had the ability to sing since songs were preserved in their minds [7]. Music promotes interaction and encourages the stimulation of listening skills, cognitive stimulation and verbal/non-verbal expression. There was a review in 2014 of 8 studies that consisted of 400 participants, and it was found that music was the best way to reduce agitation. Music therapy is also beneficial because it is a non-pharmacological intervention which is not harmful with no adverse side effects [7].
Dementia Strategy for United Kingdom
In February of 2009, the national dementia strategy launched in the UK. This was a 5-year plan which costed about 150 million Great British pounds (GBP) to support the strategy. In 2010, the government requested to continue the strategy called the Dementia Action Alliance (DAA) [8]. The DAA now has more than 50 organizations to ensure the strategy is in place. The aim of the strategy in the United Kingdom (UK) is to ensure there are improvements made to the dementia services in 3 areas, which include awareness, early diagnosis/intervention and high/efficient quality of care. Dementia has been a huge challenge to the United Kingdom since there are approximately 700,000 people living with dementia. The cost of dementia is 17 billion GBP a year. In 30 years, the UK will have 1.4 million PWD which will be 50 billion GBP a year [8]. There are 17 objectives’ that the dementia strategy in the UK has outlined including early diagnosis and intervention and enhancing quality of life, evidence informed care and intervention. [8].
Music & Dementia Connection
In clinical practice, pharmacological interventions include the use of antipsychotic and benzodiazepines drugs. These drugs help treat the behavioural and psychological symptoms of the disorder. While there is some evidence of efficacy, there are side effects such as reduction in cognitive ability, extrapyramidal symptoms and confusion. These side effects are frequent with the use of antipsychotic drugs. Nonpharmacological interventions should be considered first for the treatment of BPSD since they seek to minimize symptoms [9]. The use of nonpharmacological interventions has resulted in many benefits for persons with dementia as it increases the quality of life, reduces agitation and depression. There are many different types of non-pharmacological interventions and music therapy is one of them.
Music therapy has been effective in significantly reducing aggressiveness and anxiety. The use of songs can change the focus of attention and prompt positive memories from a person’s past which can help alleviate agitation. It is found that effective results are derived from personalized activities which are tailored according to the participants interests, abilities and skills [9]. Five studies have analyzed how effective non-pharmacological activities are in managing BPSD. De Oliveria et al. investigated an intervention called Tailored Activity Program (TAP). TAP is focused on reducing agitated behaviour and other behavioral issues associated with dementia through a selection of activities that are tailored according to the patients’ needs and interests. This program was offered to caregivers for increased self-efficacy. It was found that BPSD such as agitation, repetitive questioning, arguments and other forms of behaviours such as spitting, and yelling were reduced through the music activity. The human memory has a process to code, store and retrieve. Musical memory has a neural coding that stores musical experiences. A study conducted by Jacobsen et al investigated music and people with dementia. Jacobsen et al found that music was preserved in the patient’s minds, and musical memory is partially independent from the other memory systems. Although other functions of the brain are impaired by dementia, music memory remains intact [10].
Music engages many parts of our brain such as temporal, frontal, parietal, cerebral and limbic systems. It affects semantic memory, motor and rhythm. Music plays a prominent role in communication, social interaction, emotional self-regulation and most importantly aging. Music enhances attention, memory and cognitive functioning. It contributes to positive aging by reduced social seclusions, increased emotional well-being and maintenance of competence. Music helps to reduce anxiety and improve cognitive thinking. It is effective in alleviating symptoms for dementia such as agitation, anxiety, depression and cognitive thinking [11]. Music has been found to improve the quality of life for people with dementia (PWD). It improves mood, enhances attention, orientation and function by playing old songs which triggers part of the long-term memory [12].
Music Therapy and Personalized Music Intervention
Music is a form of non-pharmacological intervention that can help to alleviate symptoms of dementia and increase the quality of life which motivates and excites patients. It may trigger memories, movements and positive emotions for those affected by dementia. Music facilitates speech reconstruction, improvement in articulation and breathing. Patients who can no longer speak can sometimes sing to familiar songs and express their feelings, which reduces the risk of dementia and decline in cognitive functioning [12]. Personalized Music Intervention (PMI) is a safe and inexpensive way of improving mood, behaviour and the quality of life for individuals with dementia. Researchers have found that a personalized music listening program led to more than half of patients showing mood improvements. Personalized music depends on the intervention and the tools vary accordingly such as headphones, iPod or CD players. These are the tools that can be used to personalize music intervention along with various songs from different time periods [12].
Behavioral and Psychological Symptoms of Dementia
Behavioral and psychological symptoms of dementia (BPSD), also known as neuropsychiatric symptoms. include depression, hallucinations, agitation, aggression, anxiety and irritability, sexual disinhibition. It has been found that approximately 90% of people with dementia have BPSD. BPSD causes distress to patients, and increases health care costs, long term hospitalization and the misuse of medications. People with dementia may have more than one BPSD symptom. The pathogenesis of BPSD has not been clearly identified, but is probably caused by social, biological and psychological factors [13].
The clinical manifestation of BPSD is connected to genetic factors, neurochemical and neuropathological roles. BPSD affects people with dementia through an emotional experience, motor function, thoughts and perception. The symptoms of depression occur frequently, and patients may be unable to express feelings such as sadness, unhappiness and low self-esteem. They may be preoccupied with depressing topics and hopelessness. The more prominent symptoms are anhedonia, somatic concerns, panic, apprehension and physical and motor tension. Apathy can be mistaken for depression as both of these symptoms diminish interest, possess a lack of interest and energy [13].
When severe dementia is associated with depression, delusional thoughts may also be present such as guilt, persecution and worthlessness. Disturbances in motor function can be observed through less or more of motor activity which does not have to be associated with abnormalities within motor function [13]. Appetite change is common as dementia patients lose weight due to hypermetabolism and inflammatory issues which is connected to hormonal disturbances [13]. BPSD requires an assessment of neuropsychiatric symptoms which collects information about objective behaviour, clinical history and subjective experience. Some abnormal symptoms cannot be obtained through a clinical assessment; therefore, a family member or caregiver would be able to give information that is essential in obtaining neuropsychiatric abnormal disturbances. It is crucial to promote early interventions to avoid neuropsychiatric symptoms and avoid the need for crisis-based interventions [13].
BPSD is common in dementia regardless of the stage. The frequency of BPSD can vary depending on the setting and population. Neuropsychiatric symptoms occur in about 35-85% of people with dementia who have mild impairment and are less frequent in a community dwelling compared to patients who are in a hospital setting or a long-term care facility [13]. Those that experience mood and psychotic changes can shortened prognosis and poorer outcomes, psychosis is associated with an increase in mortality and cognitive declines [13]. It has been found that depressive symptoms have been linked to the progression of dementia, affecting up to 46% of patients who have dementia [13]. BPSD can lead to poor quality of life and distress in individuals with dementia and their caregivers. BPSD has a physical and psychological impact on caregivers. A caregiver dedicates a lot of time directly to managing the manifestation of BPSD which contributes to a need for hospitalization or placement in a long-term care (LTC) facility. Placement in LTC then confers increases in the direct and indirect costs associated with dementia and BPSD. Psychotic and disruptive behaviors are the most burdensome to the caregivers.
Statistics and Trends
Dementia is the leading cause of mortality and morbidity in the Western countries with the prevalence of dementia expected to triple by 2050, due to the aging population. It has been estimated that 24.3 million people have dementia and there are 4.6 million new cases annually [14]. The number will be doubled every 20 years and it is expected to reach 82 million in 2030 and 152 million people in 2050. This is due to people who are living with dementia in low to middle income countries. The estimated proportion of the population aged 60 and over is between 5-8%. There are 50 million people worldwide who are affected with dementia and 10 million new cases each year [4]. There is a new case of dementia every 3 seconds in the world. It is predicted that there will be 114 million people with dementia worldwide. Majority of the people with dementia live in developing countries which accounts for 60% of PWD. This will increase to 71% by 2040. The number of people with dementia in developing areas are predicted to be three to four times higher than in developed regions. The Global Burden of Disease estimated 11.2% of people around the world with dementia aged 60 or more which is higher than stroke. Currently there are roughly 56,000 Canadians with dementia in hospitals which is not the ideal situation [14].
Dementia is most commonly diagnosed after age 65. However, in Ontario 7% of diagnosis are made for people between 40 and 65 years of age, and 64% of them are women [6]. It is important to spread awareness and understand dementia to challenge the misconceptions about this condition [15]. Alzheimer’s disease is a common form of dementia and it affects 60-70% of the cases. Dementia accounts for majority of the disability and dependency worldwide which impacts the economy, carers, families and society. The physical, psychological and social impact affects the patients with dementia. In Canada, there are more than 419,000 Canadians over the age of 65 who are living with dementia. It has been estimated that BPSD affects 90% of people with dementia which is associated with poor outcomes which includes long term hospitalization, increased health care cost, misuse of pharmacological interventions and distress amongst patients and caregivers [16]. In Ontario, there are 200,000 people who are living with dementia and the number will increase as the population ages. This number will rise to 255,000 in 2020, and there will be over 430,000 people with dementia by 2038 [6].
Globally there are 50 million people living with dementia, and 5.2% of people over the age of 60 have been diagnosed with dementia globally. The number of people living with dementia will increase to 152 million people globally in 2050 which is a 204% increase from 2018. There are 58% people living with dementia in low to middle income countries which will increase to 68% by 2050. East Asia has 9.8 million people diagnosed with dementia, Western Europe has 7.5 million people, and North America has 4.8 million people. The number of people with dementia in Western Europe is expected to increase from 7.5 million to 14.3 million by 2050 [17].
The prevalence rate of dementia is affected by the amount of education that has been acquired by an individual. A study shows that people who attain a higher education have a lower chance to get dementia, and people with no education have a higher chance to get dementia due to poor cognitive functioning [18]. Dementia is the 5th leading case of mortality in the world. The impact to the health care system is significant since PWD are the largest users of health care. Generally, older people need more care and attention due to multiple health conditions which burdens the health care system [19]. Other key findings include that about 1 in 4 seniors aged 85+ above have been diagnosed with dementia. The prevalence for dementia doubles every 5 years for Canadians 65 and above [20].
Health Care Cost of Dementia
The health care cost of one person with dementia including medical care and nursing home costs approximately $41,689 and $56,290 which is mainly driven by social care needs and health care [21]. In 2011, care providers provided 19.2 million unpaid hours that were used towards dementia care and this will double by 2031 [2]. The total cost for dementia in 2010 was $604 billion which is equivalent to 1% of the world’s gross domestic product. The cost is set to soar worldwide to an 85% increase in costs by 2030 [19]. As of 2016, the health care cost and out of pocket cost is estimated at 10.4 billion per year. By 2031, there will be an increase by 60% which will account for 16.6 billion [5]. Dementia is a growing public health concern and it will account for 33 billion dollars annually in health care cost. It has been estimated that there will be more than 152 million people living with dementia worldwide with the cost of 325 billion from the year 2008-2038 [6]. BPSD alone will account for 30% of all direct health care costs [16].
The cost of dementia worldwide was estimated at 604 billion US [19]. In 2016 the global estimate of dementia was 948 billion, and now the current global cost of dementia is 818 billion [19]. In 2050 the cost of dementia will rise to 1.1 trillion. In 2019 the caregivers will provide an estimate of 18.5 billion hours of care which is valued at 234 billion. The cost of a caregiver taking care of a patient diagnosed with dementia is estimated at $350,174 [22]. In 2013, approximately 40 million family members provided 37 billion hours of care which is worth 470 billion unpaid care. Family caregivers spend approximately $6,954 out of pocket for dementia [23]. Nationally in 2019 the cost of caring for someone with moderate dementia is $4,650 per month [24]. Caregivers give 26 hours per week of informal care compared to 17 hours. It has been reported that 45% of unpaid caregivers of seniors are more likely to experience distress than other caregivers [25]. In Canada it was reported that 1.4 billion was the estimated out of pocket cost for caregivers in Canada in 2016. This will rise to 2.4 billion in 2031 [25].
Study Objective
The objective of this research is to examine the literature on the impact of music therapy on dementia patients.
Methods
Peer reviewed articles were found through electronic databases which include Ovid Medline, CINAHL, and PsycINFO. Randomized control trials were used in the search engine for the study. The population that was included in the study was from ages 65-80 males and females from Ontario, Canada. The search terms that were used were music, music therapy; dementia or dementia disease; hospital admission and aged hospital patient; music intervention or personalised music intervention; seniors, elderly or aged 65+; hospital admission or aged hospital admission. The literature search was for articles dated from January 2000 until present August 2019. The studies selected for the inclusion criteria were peer reviewed articles with an abstract pool and full articles published in English. The inclusion criteria also included research articles on dementia patients in the long terms care facility, nursing homes and care giver homes. The grey literature was also searched for additional information on dementia, incidence/prevalence and statistics. The sites used for grey literature were the World Health Organization, Alzheimer’s Association, Canadian Institute for Health Information, Alzheimer’s Society of Canada and the Government of Canada and Ontario site. The exclusion criteria to the search strategy was non-English and non-peer reviewed articles. Editorials, letters, guidelines, patient testimonials were excluded. Further exclusion criteria included target population under 65 and patients with dementia.
Flowchart of Literature Search Process
The extraction of selected studies was based on review of abstracts. The rest of the information from the study was determined by the inclusion criteria. Data extraction was performed by a single reviewer. Extracted information included study design, population, sample size, music-based intervention, outcome, result, method and conclusion. The quality of the study was assessed using the Cochrane RoB 2.0 (Risk of Bias) Tool.
Results
In brief, the screening located 968 potential sources of which 129 were redundant articles. There were a total of 55 articles that met the inclusion criteria and 20 articles were selected. A ranking system of 8 levels was used to justify the strength of the article. Level I is the highest ranking which is a systematic review of a randomized control trial, or meta-analysis. Level II is a single, blinded RCT. Level III is a systematic review of correlational or longitudinal studies. Level IV includes a longitudinal or correlational study. Level V is a systematic review of descriptive or qualitative studies. Level VI consists of a single physiological, qualitative or descriptive study. Level VII is the lowest ranking which consists of opinions of other experts, panels or communities [26].
Table 2: Summary Results Chart on the Effects of Music on Dementia.
|
Author (s), year & Country |
Methodology |
Research Findings |
Rank |
|
Garland K, Beer E, Eppingstall B, O’Connor DW (2007) Australia [27] |
30 nursing home residents had behavioral issues related to dementia. This was a randomized single blind exposure of 15 min audiotapes from a stimulated family member, music, and a placebo reading condition from horticultural text. Multiple behaviors were counted and absent at regular intervals. All 3 treatments were compared to usual care. |
Stimulated music and preferred music were effective in reducing agitated behavior. The response varied widely.
The simplest technology can improve lives of patients and their caregivers |
II |
|
Cohen-Mansfield J, Marx M, Dakheel-Ali M, Thein K. (2015) USA [28]
|
There were 89 nursing home residents from 6 nursing home in Maryland. The mean age was 85.9 years. Research Assistants had tailored interventions according to the participants needs. The effects of the intervention were noted immediately by the research assistant. Each participant was observed for 3 days every half hour between 8 am to 9 pm. Each observation was 3 minutes. |
The intervention with the highest impact on behavior was music, folding towels, hand massage, care and videos.
|
IV |
|
Gerdner LA (2000) USA [29] |
There were 39 participants from 6 long term care facilities in Lowa. The sample consisted of 30 women and 9 men. The mean age was 82 years. Baseline data was collected in 3 weeks. A modified Hartsock music preference questionnaire guided the section of personal music. Group A consisted of 16 participants who received an individualized music intervention for 6 weeks, following a 2-week washout period and 6 weeks of classical relaxation music. Group B consisted of 23 participants in the same protocol, but the order was reversed.
The intervention was for 30 mins, 2 times per week |
The Bonferroni post hoc showed a significant reduction in agitation during individualized music, in comparison to classical. |
IV |
|
Park H, Specht P (2009) USA [30] |
This study investigated the effects of music on patients with dementia at home. 15 individuals listened to their preferred music for 30 mins prior to when patients feel agitated 2 times per week for 2 weeks with no music intervention for the next 2 weeks. This was repeated once. |
The mean agitation level was significantly reduced while patients were listening to music than before listening to music. |
IV |
|
McDermott O, Orrell M, Ridder MH (2013) London [31] |
There was a focus group and an interview was conducted with home care residents, hospital patients with dementia, home care staff, and music therapist. 6 key themes were identified and applied in these 4 areas. The findings of the analysis were investigated to develop a theoretical model on music. The aim of the focus group/interview was to engage the participants in a musical experience. The questions that were asked was “What does music mean to you? What do you think of your music therapy/music activities? If music is important to you, in what way? (People with dementia).” “What changes and responses do you observe in your family members/clients following music therapy or music activities? How do you know when music is meaningful to the person? (Families, staff and music therapists)”.
|
The psychosocial model was developed. Theme 1: The accessibility of music. All participants seemed interested in music by feet tapping, clapping or singing along. People with dementia had immediately responded to it. The residents and hospital patients explained singing and listening to music was emotionally meaningful. Theme 2: Retained memory of song lyrics connected to personal history. Music brings back memories, it is a personal and cultural identity
Theme 3: Connected, a new experience of music making. Participants took interest in learning how to play music
Theme 4: Effects of music on mood. Music helped to improve mood and decrease agitation levels. Everyone had a brighter mood.
Theme 5: Effects of music on home care environment. Music had an effect on visiting family members.
Theme 6: Evaluation and communication of music therapy
The effects of music are beyond the reduction of behavioral and psychological symptoms. Music was seen to maintain and improve the quality of life. It was also evident that music was preserved in the minds of dementia patients. |
V |
|
Poli LF, Bieleninik L, Brondino N, Chen X, Gold C (2017) London [32] |
A systematic review was conducted, and a search was performed in Medline, PsycINFO, Embase, CINAHL and RILM. All RCTs that had a comparison between music therapy, standard care and non-musical interventions were included. The purpose was to evaluate cognitive outcomes. |
There were 1089 records, 110 were assessed for eligibility and 7 met the inclusion criteria. Music therapy patients were involved in the production of music. Music enhanced the frontal cortex part of the brain. It is related to improvement in memory. |
I |
|
Guétin S, Portet F, Picot MC, Pommié C, Messaoudi M, Djabelkir L, Touchon J (2009) [33]
|
This was a single centered randomized control trial which was comparative in nature. It was a blinded assessment. The follow up time period was 24 weeks. The treatment group had 15 participants who had a weekly session of receptive music therapy. The musical style was chosen by patients. The control group which also consisted of 15 participants were in the same reading sessions. The principle endpoint was measured at 1,4,8,16 and 24 weeks. Anxiety was measured and depression was analyzed as the secondary end point. |
There was significant improvement in anxiety and depression from the music therapy group from week 4 until 16. The effect was sustained for 8 weeks after the session had ended between week 16 and 24.
These results state that music is an effective therapy on depression and anxiety patients. |
II |
|
Van de Winckel, A, Fey H, De Weerdt W, Dom R (2004) Belgium [34] |
This is a randomized control trial which took place in a Belgium hospital. There were 25 patients with dementia. 15 patients had attended an exercise training for 3 months supported by music for 30 mins per session. The participants were compared with 10 control patients who received equal attention by a daily conversation.
Cognition was measured using Mini Mental Sate Examination and behavior was evaluated through Stockton Geriatric Rating Scale. |
The exercise group with the music had shown improvement in cognition. Music based exercise program was effective for patients with moderate to severe dementia. |
IV |
|
Ying Y, Yanzhen W, Yulei S, Yamei B (2019) China [35]
|
A randomized control trial was conducted on the effects of music therapy on dementia patients. The English and Chinese databases were searched, and a Meta-Analysis was performed with a RevMan 5.3. |
13 articles were included with 580 patients. The meta-analysis had indicated a significant improvement in anxiety and depressive symptoms in the intervention group than the control group after the intervention. Music therapy improves anxiety and depressive symptoms of patients with dementia. |
I |
|
Leva V, Guy M (2013) Sweden [36] |
This is a meta-analysis on the effects of music on dementia patients. All original studies found with the key words “music and dementia”. |
There were 19 studies with 478 patients. All patients had indicated a significant positive effect on behavioral, physiological and cognitive outcome. Music intervention are effective and have a potential to increase the quality of life. |
I |
|
Watanabe K, Torikawa S, Shiota K, Matsui H, Shigenobu K. & Ikeda M (2003) Japan [37]
|
The effects of music were investigated on dementia patients with Alzheimer’s and vascular disease. Participants Ss had 6 males and 27 females with Alzheimer’s disease; 7 males and 10 females had vascular disease. The mean age was 79.9. Ss had weekly sessions for music therapy for 2 months. The sessions were evaluated using the Ehime Music Therapy scale. |
The results indicated that speech and social activities had increased as participants became familiar with the therapeutic activities and staff members. Singing was easy for the Ss group and comprehension improved by utilizing some musical devices. Music therapy induced physical movements and was more effective than other activities. |
IV |
|
Lyu J, Zhang J, Mu H, Li W, Champ M, Xiong Q, Li M (2018) China [38]
|
There was a total of 298 patients diagnosed with Alzheimer’s. The participants were divided based on the severity of dementia.
Participants were divided into 3 groups which was a singing group, lyric group and control group. These groups had received an intervention for 3 months. Participants underwent a series of tests related to cognitive functions, daily living activities and neuropsychological symptoms. |
Music therapy is more effective for improving psychiatric symptoms and verbal fluency. An analysis shows that music therapy is great for enhancing memory and language. Overall music therapy is a good tool to enhance cognitive function and mental well-being. This is a good first line of treatment for Alzheimer’s and dementia patients. |
II |
|
Tuet R W K, Lam L C W (2006) Hong Kong [7] |
There were 14 patients with dementia who had at least one type of agitated behavior. Participants were put into 2 groups. 1 group received music therapy, and the other group did not receive music therapy with usual care for 3 weeks. The groups were crossed over after 3 weeks for the active and control intervention for another 3 weeks. Behavioral disturbances were measured by Cohen-Mansfield Agitation and neuropsychiatric inventory. |
There was a reduction in the Cohen-Mansfield Agitation and neuropsychiatric inventory scores. The reduction was not found in usual care. There was no lasting effect in both groups. The results show that music has a positive effect on behavioral disturbances. |
IV |
|
Svansdottir H B, Snaedal J (2006) Iceland [39] |
This was a case control study carried out by music therapist in 2 nursing homes and psychogeriatric wards. There were 38 patients diagnosed with Alzheimer’s who were assigned to a random music therapy group and control group. |
There was a reduction in activity disturbances during the 6 weeks’ time period such as aggressiveness and anxiety. This was rated through the Behavior Pathology in Alzheimer’s Disease Rating Scale (BEHAVE-AD). Music therapy was found to be a safe and effective method for treating anxiety and agitation. |
IV |
|
Lin Y, Chu H, Yang C, Chen C, Chen S, Chang H, Chou K (2011) Taiwan [40]
|
This was an experimental design for participants suffering from dementia who reside in nursing facilities.
49 people were in the experimental group and 51 in the control group. The experimental group participated in a music intervention for 12 sessions that were 30 minutes long. This was conducted twice a week for 6 weeks. The control group carried out normal daily activities.
|
The music intervention experimental group showed an improved performance at the 6th and 12th session. 1 month after the therapy, there was a reduction in agitation, non-aggressive verbal and physical behavior. It is essential for nursing facilities to incorporate music interventions in order to reduce agitation and emotionally relax patients with dementia. |
II |
|
Palisson J, Roussel-Baclet C, Maillet D, Belin C, Ankri J, & Narme P (2015) [41]
|
12 patients had mild Alzheimer’s and 15 healthy controls learned texts which was either musical which is sung, or non-musical association, which is a silent movie sequence, or without association which is spoken alone. |
Results showed that music which was sung was more helpful to retain in memory than spoken texts. The musical experience was robust and had a good impact on Alzheimer’s patients. The non-musical experience was helpful but to a lesser extent. A musical association facilitates learning and retention for patients with Alzheimer’s. |
IV |
|
Lou M (2001) [42]
|
This paper describes the use of music to decrease agitated behavior. 7 articles were assessed through online databases. The databases searched were CINAHL and Medline. The key words were music therapy, demented elderly and agitated behavior. |
Music interventions was seen to decrease agitated behaviors. 4 of the studies used background music, 3 studies used preferred music. Amongst all of these studies, 6 studies had a positive impact on reducing agitated behavior, and 1 study shows no significant difference. The findings were consistent and suggested that music is a great way to decrease BPSD. |
I |
|
Choi A, Lee M, Cheong J, Lee J (2009) South Korea [43] |
20 patients were allocated to a music intervention group or a usual care group. The music intervention group received music therapy 50 minutes a day, 3 times per week for 5 weeks. |
After 15 sessions, the music intervention group improved in agitation, behavioral and psychological symptoms. |
II |
|
Sakamoto M, Ando H, Tsutou A (2013) Cambridge [44]
|
39 participants who were diagnosed with severe Alzheimer’s were randomly assigned to 2 passive music intervention groups. The third group is a non-music control group (non-intervention control group). All 3 interventions were performed for 30 minutes, once a week consecutively for 10 weeks. The effects after the intervention was evaluated using an emotional and stress response which was measured by autonomic nerve index and face scale. BPSD changes were evaluated using BEHAVE-AD rating scale. |
The 2 passive music intervention groups caused a short-term parasympathetic dominance. The interactive intervention in the music groups had the greatest improvement in emotions. There was a reduction in BPSD. Interactive music sessions can store cognitive and emotional function, reduce stress and improve the quality of life. |
IV |
Gaps in the Literature
Several studies in the literature have examined music intervention and music therapy as shown in the results. They looked at music therapy conducted by music therapist or health care professionals. The incomplete aspect of this review is the use of Personalized Music Intervention (PMI). There is limited research of PMI on dementia in the long-term care, nursing and caregiver homes. PMI is a safe and inexpensive way for improving mood, behaviour and the quality of life for PWD. The tools vary accordingly such as headphones, iPod or CD players. These are the tools that can be used to personalize music intervention along with various different songs from different times [12].
Conclusion
Dementia is one of the leading causes of death amongst the geriatric population with no cure. Since there is no cure, medical professionals can aim to reduce BPSD and utilize interventions such as a non-pharmacological intervention to help patients with dementia. Nonpharmacological interventions are beneficial due to the lack of side effects. This intervention uses music therapy which is widely used to reduce symptoms such as BPSD, stress and anxiety. It increases the quality of life and decreases the symptoms of BPSD’s. PMI is a safe and inexpensive way for improving mood, behaviour and the quality of life [12]. It is a non-pharmacological approach that utilizes music to help treat patients with a clinical condition or disorder. This intervention will encourage patients to connect with their past and improve their quality of life by selecting their own music.
The findings of this review are important from a practical point of view because there are many patients suffering from dementia in the long-term care facilities, care giver homes and hospitals. Additionally, since there are limited studies on the effects of PMI on dementia, this study adds to the scholarly literature by qualifying PMI to improve mood, behavior and the quality of life. The specific importance of individual preference and recognitions of music in a non-supported music environment is identified. PMI improves overall health because it reduces stress, depression, emotional/behavioral issues within dementia. Quality of life will improve, and this may reduce the burden on the health care system as well as the cost associated with dementia.
Future Directions for Research
It is preferable to use personalized music therapy in the earlier stages to avoid BPSD symptoms as dementia progresses. For future studies, it is recommended that study designs increase their sample sizes for accurate results and have a broader spectrum of patients to compare. As the use of music is prevalent in everyday living, it is beneficial amongst people with dementia. It is important to gain an understanding of how music is able to reach those with advanced levels of cognitive decline, and to develop protocols that take music taste into account, and the symptoms that the music is being used to address. It is encouraged for researchers to conduct a design in which conditions are matched and seek to overcome the limitations and issues discussed in this paper.
Article Info
Article Type
Review of LiteraturePublication history
Received: Sun 19, Jan 2020Accepted: Fri 31, Jan 2020
Published: Mon 10, Feb 2020
Copyright
© 2023 Wally J. Bartfay. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GGR.2019.01.04
Author Info
Andra Duff-Woskosky Julie Earle Marina Ali Sheri Horsburgh Wally J. Bartfay
Corresponding Author
Wally J. BartfayFaculty of Health Sciences, Ontario Tech University, Canada
Figures & Tables
Table 1: Definitions of Key Terms.
|
Key Terms |
Definitions |
Reference |
|
Dementia |
Dementia is defined as the deterioration in memory, behavior, cognitive thinking and the inability to conduct everyday basic activities. It is a chronic progressive neurological disorder. Dementia is associated with emotional and behavioral problems which also decrease the quality of life. |
WHO, (2019) [4] |
|
Alzheimer’s Disease (AD) |
AD is the most common form of dementia that causes problem with the memory function, cognitive thinking, and behavior. Symptoms progress overtime and get severe enough to affect the daily tasks and function. |
Alzheimer’s Association, (2019) [22] |
|
Vascular dementia (VD) |
VD is the second most common form of dementia. It is described as a set of symptoms that include issues with problem solving/language, memory loss and cognitive issues. This is caused by brain damage which develops after a stroke and blocks the arteries in the brain blocking the blood flow. When blood flow is impaired, it is possible for the blood vessels to be damaged with reduced circulation. |
Mayo Clinic, (2019) [48] |
|
Lewy Bodies (LB) |
LB is a form of dementia which is associated with a protein called alpha-synuclein. This is an abnormal deposit that affects the chemicals in the brain and leads to problems with movement, mood, behavior and thinking. |
NIH, (2019) [49] |
|
Frontotemporal Dementia (FD) |
FD is a group of disorders which is a form of dementia. It causes progressive nerve cell loss in the frontal lobe or temporal lobe of the brain. This leads to a deterioration in behavior, personality issues and difficulty in comprehending language. |
Alzheimer’s Association, 2019 [22] |
|
Music |
Music is an art and expression of emotions. “It is the art of ordering or sounds in succession, in combination, and in temporal relationships to produce a composition having unity and continuity” |
Merriam-Webster, 2019 [45] |
|
Music Intervention (MI) |
MI is defined as a therapeutic setting where music is controlled to accomplish a psychological, physiological and emotional well-being during a treatment of a disease. |
Pedersen et al. (2017) [46] |
|
Music Therapy (MT) |
MT is a music intervention that is used to accomplish therapeutic goals of individuals by a professional who has completed a music therapy program. It addresses physical, cognitive, emotional and social needs. Music therapy helps people express themselves when avenues of communication are difficult. |
American Music Therapy Association [AMTA], (2019) [47] |
|
Personalized Music Intervention (PMI) |
PMI is a non-pharmaceutical approach which utilizes music to help treat patients who have a clinical condition and disorder. Some symptoms include depression, anxiety, agitation and dementia. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
|
Behavioral and Psychological Symptoms of Dementia (BPSD) |
BPSD, also known as neuropsychiatric symptoms, represents a group of cognitive symptoms and behavior occurring in patients with dementia. BPSD is common in dementia irrespective of the subtype. BPSD includes, hallucinations, agitation, violent motor behavior, anxiety and irritability. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
|
Pharmacological Intervention (PI) |
PI is the use of a variety of medication to treat BPSD and other effects of dementia such as the symptom’s and side effects. The medications include antidepressants, AChEI, mood stabilizers, typical and atypical antipsychotics, benzodiazepines, memantine and other drugs. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13]
|
|
Nonpharmacological Intervention (NI) |
NI is the use of therapies excluding medications to improve the quality of life for patients with dementia. The therapy interventions are classified into various different categories. This includes cognitive/emotion-oriented intervention such as stimulated presence therapy, reminiscence therapy and validation therapy. Sensory stimulation includes light therapy, music therapy, aromatherapy and acupuncture. Behavior management technique and psychological intervention such as exercise and animal-assisted therapy. |
Cerejeira, Lagarto & Mukaetova-Ladinska, (2012) [13] |
Table 2: Summary Results Chart on the Effects of Music on Dementia.
|
Author (s), year & Country |
Methodology |
Research Findings |
Rank |
|
Garland K, Beer E, Eppingstall B, O’Connor DW (2007) Australia [27] |
30 nursing home residents had behavioral issues related to dementia. This was a randomized single blind exposure of 15 min audiotapes from a stimulated family member, music, and a placebo reading condition from horticultural text. Multiple behaviors were counted and absent at regular intervals. All 3 treatments were compared to usual care. |
Stimulated music and preferred music were effective in reducing agitated behavior. The response varied widely.
The simplest technology can improve lives of patients and their caregivers |
II |
|
Cohen-Mansfield J, Marx M, Dakheel-Ali M, Thein K. (2015) USA [28]
|
There were 89 nursing home residents from 6 nursing home in Maryland. The mean age was 85.9 years. Research Assistants had tailored interventions according to the participants needs. The effects of the intervention were noted immediately by the research assistant. Each participant was observed for 3 days every half hour between 8 am to 9 pm. Each observation was 3 minutes. |
The intervention with the highest impact on behavior was music, folding towels, hand massage, care and videos.
|
IV |
|
Gerdner LA (2000) USA [29] |
There were 39 participants from 6 long term care facilities in Lowa. The sample consisted of 30 women and 9 men. The mean age was 82 years. Baseline data was collected in 3 weeks. A modified Hartsock music preference questionnaire guided the section of personal music. Group A consisted of 16 participants who received an individualized music intervention for 6 weeks, following a 2-week washout period and 6 weeks of classical relaxation music. Group B consisted of 23 participants in the same protocol, but the order was reversed.
The intervention was for 30 mins, 2 times per week |
The Bonferroni post hoc showed a significant reduction in agitation during individualized music, in comparison to classical. |
IV |
|
Park H, Specht P (2009) USA [30] |
This study investigated the effects of music on patients with dementia at home. 15 individuals listened to their preferred music for 30 mins prior to when patients feel agitated 2 times per week for 2 weeks with no music intervention for the next 2 weeks. This was repeated once. |
The mean agitation level was significantly reduced while patients were listening to music than before listening to music. |
IV |
|
McDermott O, Orrell M, Ridder MH (2013) London [31] |
There was a focus group and an interview was conducted with home care residents, hospital patients with dementia, home care staff, and music therapist. 6 key themes were identified and applied in these 4 areas. The findings of the analysis were investigated to develop a theoretical model on music. The aim of the focus group/interview was to engage the participants in a musical experience. The questions that were asked was “What does music mean to you? What do you think of your music therapy/music activities? If music is important to you, in what way? (People with dementia).” “What changes and responses do you observe in your family members/clients following music therapy or music activities? How do you know when music is meaningful to the person? (Families, staff and music therapists)”.
|
The psychosocial model was developed. Theme 1: The accessibility of music. All participants seemed interested in music by feet tapping, clapping or singing along. People with dementia had immediately responded to it. The residents and hospital patients explained singing and listening to music was emotionally meaningful. Theme 2: Retained memory of song lyrics connected to personal history. Music brings back memories, it is a personal and cultural identity
Theme 3: Connected, a new experience of music making. Participants took interest in learning how to play music
Theme 4: Effects of music on mood. Music helped to improve mood and decrease agitation levels. Everyone had a brighter mood.
Theme 5: Effects of music on home care environment. Music had an effect on visiting family members.
Theme 6: Evaluation and communication of music therapy
The effects of music are beyond the reduction of behavioral and psychological symptoms. Music was seen to maintain and improve the quality of life. It was also evident that music was preserved in the minds of dementia patients. |
V |
|
Poli LF, Bieleninik L, Brondino N, Chen X, Gold C (2017) London [32] |
A systematic review was conducted, and a search was performed in Medline, PsycINFO, Embase, CINAHL and RILM. All RCTs that had a comparison between music therapy, standard care and non-musical interventions were included. The purpose was to evaluate cognitive outcomes. |
There were 1089 records, 110 were assessed for eligibility and 7 met the inclusion criteria. Music therapy patients were involved in the production of music. Music enhanced the frontal cortex part of the brain. It is related to improvement in memory. |
I |
|
Guétin S, Portet F, Picot MC, Pommié C, Messaoudi M, Djabelkir L, Touchon J (2009) [33]
|
This was a single centered randomized control trial which was comparative in nature. It was a blinded assessment. The follow up time period was 24 weeks. The treatment group had 15 participants who had a weekly session of receptive music therapy. The musical style was chosen by patients. The control group which also consisted of 15 participants were in the same reading sessions. The principle endpoint was measured at 1,4,8,16 and 24 weeks. Anxiety was measured and depression was analyzed as the secondary end point. |
There was significant improvement in anxiety and depression from the music therapy group from week 4 until 16. The effect was sustained for 8 weeks after the session had ended between week 16 and 24.
These results state that music is an effective therapy on depression and anxiety patients. |
II |
|
Van de Winckel, A, Fey H, De Weerdt W, Dom R (2004) Belgium [34] |
This is a randomized control trial which took place in a Belgium hospital. There were 25 patients with dementia. 15 patients had attended an exercise training for 3 months supported by music for 30 mins per session. The participants were compared with 10 control patients who received equal attention by a daily conversation.
Cognition was measured using Mini Mental Sate Examination and behavior was evaluated through Stockton Geriatric Rating Scale. |
The exercise group with the music had shown improvement in cognition. Music based exercise program was effective for patients with moderate to severe dementia. |
IV |
|
Ying Y, Yanzhen W, Yulei S, Yamei B (2019) China [35]
|
A randomized control trial was conducted on the effects of music therapy on dementia patients. The English and Chinese databases were searched, and a Meta-Analysis was performed with a RevMan 5.3. |
13 articles were included with 580 patients. The meta-analysis had indicated a significant improvement in anxiety and depressive symptoms in the intervention group than the control group after the intervention. Music therapy improves anxiety and depressive symptoms of patients with dementia. |
I |
|
Leva V, Guy M (2013) Sweden [36] |
This is a meta-analysis on the effects of music on dementia patients. All original studies found with the key words “music and dementia”. |
There were 19 studies with 478 patients. All patients had indicated a significant positive effect on behavioral, physiological and cognitive outcome. Music intervention are effective and have a potential to increase the quality of life. |
I |
|
Watanabe K, Torikawa S, Shiota K, Matsui H, Shigenobu K. & Ikeda M (2003) Japan [37]
|
The effects of music were investigated on dementia patients with Alzheimer’s and vascular disease. Participants Ss had 6 males and 27 females with Alzheimer’s disease; 7 males and 10 females had vascular disease. The mean age was 79.9. Ss had weekly sessions for music therapy for 2 months. The sessions were evaluated using the Ehime Music Therapy scale. |
The results indicated that speech and social activities had increased as participants became familiar with the therapeutic activities and staff members. Singing was easy for the Ss group and comprehension improved by utilizing some musical devices. Music therapy induced physical movements and was more effective than other activities. |
IV |
|
Lyu J, Zhang J, Mu H, Li W, Champ M, Xiong Q, Li M (2018) China [38]
|
There was a total of 298 patients diagnosed with Alzheimer’s. The participants were divided based on the severity of dementia.
Participants were divided into 3 groups which was a singing group, lyric group and control group. These groups had received an intervention for 3 months. Participants underwent a series of tests related to cognitive functions, daily living activities and neuropsychological symptoms. |
Music therapy is more effective for improving psychiatric symptoms and verbal fluency. An analysis shows that music therapy is great for enhancing memory and language. Overall music therapy is a good tool to enhance cognitive function and mental well-being. This is a good first line of treatment for Alzheimer’s and dementia patients. |
II |
|
Tuet R W K, Lam L C W (2006) Hong Kong [7] |
There were 14 patients with dementia who had at least one type of agitated behavior. Participants were put into 2 groups. 1 group received music therapy, and the other group did not receive music therapy with usual care for 3 weeks. The groups were crossed over after 3 weeks for the active and control intervention for another 3 weeks. Behavioral disturbances were measured by Cohen-Mansfield Agitation and neuropsychiatric inventory. |
There was a reduction in the Cohen-Mansfield Agitation and neuropsychiatric inventory scores. The reduction was not found in usual care. There was no lasting effect in both groups. The results show that music has a positive effect on behavioral disturbances. |
IV |
|
Svansdottir H B, Snaedal J (2006) Iceland [39] |
This was a case control study carried out by music therapist in 2 nursing homes and psychogeriatric wards. There were 38 patients diagnosed with Alzheimer’s who were assigned to a random music therapy group and control group. |
There was a reduction in activity disturbances during the 6 weeks’ time period such as aggressiveness and anxiety. This was rated through the Behavior Pathology in Alzheimer’s Disease Rating Scale (BEHAVE-AD). Music therapy was found to be a safe and effective method for treating anxiety and agitation. |
IV |
|
Lin Y, Chu H, Yang C, Chen C, Chen S, Chang H, Chou K (2011) Taiwan [40]
|
This was an experimental design for participants suffering from dementia who reside in nursing facilities.
49 people were in the experimental group and 51 in the control group. The experimental group participated in a music intervention for 12 sessions that were 30 minutes long. This was conducted twice a week for 6 weeks. The control group carried out normal daily activities.
|
The music intervention experimental group showed an improved performance at the 6th and 12th session. 1 month after the therapy, there was a reduction in agitation, non-aggressive verbal and physical behavior. It is essential for nursing facilities to incorporate music interventions in order to reduce agitation and emotionally relax patients with dementia. |
II |
|
Palisson J, Roussel-Baclet C, Maillet D, Belin C, Ankri J, & Narme P (2015) [41]
|
12 patients had mild Alzheimer’s and 15 healthy controls learned texts which was either musical which is sung, or non-musical association, which is a silent movie sequence, or without association which is spoken alone. |
Results showed that music which was sung was more helpful to retain in memory than spoken texts. The musical experience was robust and had a good impact on Alzheimer’s patients. The non-musical experience was helpful but to a lesser extent. A musical association facilitates learning and retention for patients with Alzheimer’s. |
IV |
|
Lou M (2001) [42]
|
This paper describes the use of music to decrease agitated behavior. 7 articles were assessed through online databases. The databases searched were CINAHL and Medline. The key words were music therapy, demented elderly and agitated behavior. |
Music interventions was seen to decrease agitated behaviors. 4 of the studies used background music, 3 studies used preferred music. Amongst all of these studies, 6 studies had a positive impact on reducing agitated behavior, and 1 study shows no significant difference. The findings were consistent and suggested that music is a great way to decrease BPSD. |
I |
|
Choi A, Lee M, Cheong J, Lee J (2009) South Korea [43] |
20 patients were allocated to a music intervention group or a usual care group. The music intervention group received music therapy 50 minutes a day, 3 times per week for 5 weeks. |
After 15 sessions, the music intervention group improved in agitation, behavioral and psychological symptoms. |
II |
|
Sakamoto M, Ando H, Tsutou A (2013) Cambridge [44]
|
39 participants who were diagnosed with severe Alzheimer’s were randomly assigned to 2 passive music intervention groups. The third group is a non-music control group (non-intervention control group). All 3 interventions were performed for 30 minutes, once a week consecutively for 10 weeks. The effects after the intervention was evaluated using an emotional and stress response which was measured by autonomic nerve index and face scale. BPSD changes were evaluated using BEHAVE-AD rating scale. |
The 2 passive music intervention groups caused a short-term parasympathetic dominance. The interactive intervention in the music groups had the greatest improvement in emotions. There was a reduction in BPSD. Interactive music sessions can store cognitive and emotional function, reduce stress and improve the quality of life. |
IV |
References
- Shimohama S (2017) Dementia. J Neurol Sci 381: 9.
- Government of Canada (2019) A Dementia Strategy for Canada: Together We Aspire.
- Torpy JM, Lynm C, Glass RM (2010) Dementia. JAMA 304: 1972. [Crossref]
- World Health Organization (2019) Dementia.
- Alzheimer’s Society Canada (2019) Canada’s National Dementia Strategy.
- Ontario (2019) Developing Ontario’s Dementia Strategy: Discussion Paper.
- Tuet R W K, Lam L C W (2006) A preliminary study of the effects of music therapy on agitation in chinese patients with dementia. Hong Kong J Psychiatry 16: 87-91.
- Department of Health (2013) Living well with Dementia: A National Dementia Strategy.
- De Oliveira A M, Radanovic M, de Mello P C, Buchain P C, Vizzotto A D et al. (2015) Nonpharmacological Interventions to Reduce Behavioral and Psychological Symptoms of Dementia: A Systematic Review. BioMed Res Int 2015: 218980. [Crossref]
- Moreira S V, Justi F, Moreira M (2018) Can musical intervention improve memory in Alzheimer's patients? Evidence from a systematic review. Dement Neuropsychol 12: 133-142. [Crossref]
- Sarkamo T, Tervaniemi M, Laitinen S, Numminen A, Kurki M et al. (2014) Cognitive, Emotional, and Social Benefits of Regular Musical Activities in Early Dementia: Randomized Controlled Study. Gerontologist 54: 634-650. [Crossref]
- Matthews S (2015) Dementia and the Power of Music Therapy. Bioethics 29: 573-579. [Crossref]
- Cerejeira J, Lagarto L, Mukaetova-Ladinska E B (2012) Behavioral and psychological symptoms of dementia. Frontiers Neurol 3: 73. [Crossref]
- Ferri C, Prince M, Brayne C, Brodaty H, Fratiglioni L et al. (2006) Global Prevalence of Dementia. Lancet Neurol 5: 283.
- Alzheimer’s Disease International (2019) The Global Voice on Dementia.
- Bartfay E, Bartfay W J (2013) Quality-of-Life Outcomes Among Alzheimer’s Disease family caregivers following community-based intervention. West J Nurs Res 35:98-116. [Crossref]
- Alzheimer’s Research UK (2015) Global Prevalence.
- Crimmins E, SaitoY, Kim J, Zhang Y, Sasson I, Hayward M (2018) Educational Differences in the Prevalence of Dementia and Life Expectancy with Dementia: Changes from 2000 to 2010. J Gerontol B Psychol Sci Soc Sci 73: S20-S28. [Crossref]
- World Health Organization (2015) The Epidemiology and Impact of Dementia.
- Canadian Institute for Health Information (CIHI) (2019) Dementia in Canada.
- Zhu C, Scarmeas N, Ornstein K, Albert M, Brandt Jet al. (2015) Health care use and cost in dementia caregivers: Longitudinal results from the Predictors Caregiver Study. Alzheimers Dement 11: 444-454. [Crossref]
- Alzheimer’s Association. (2019) Alzheimer’s and Dementia.
- Jenkins J (2016) Caregiving Costly to Family Caregivers. AARP.
- Dementia Care Central (2019) Alzheimer’s / Dementia Care Costs: Home Care, Adult Day Care, Assisted Living & Nursing Homes.
- Canadian institute for Health Information (CIHI) (2019) Unpaid caregiver challenges and supports.
- Bartfay W, Bartfay E (2016) Public health in Canada 2.0. 2nd edition. US: Kendall Hunt Publishing Company.
- Garland K, Beer E, Eppingstall B, O’Connor DW (2007) A comparison of two treatments of agitated behavior in nursing home residents with dementia: simulated family presence and preferred music. Am J Geriatr Psychiatry 15: 514-521. [Crossref]
- Cohen Mansfield J, Marx M, Dakheel-Ali M, Thein K (2015) The use and utility of specific nonpharmacological interventions for behavioral symptoms in dementia: an exploratory study. Am J Geriatric Psyc 23: 160-170. [Crossref]
- Gerdner LA (2000) Effects of individualized versus classical "relaxation" music on the frequency of agitation in elderly persons with Alzheimer’s disease and related disorders. Int Psychogeriatr 12: 49-65. [Crossref]
- Park H, Pringle Specht JK (2009) Effect of individualized music on agitation in individuals with dementia who live at home. J Gerontological Nurs 35: 47-55. [Crossref]
- McDermott O, Orrell M, Ridder HM (2014) The importance of music for people with dementia: the perspectives of people with dementia, family carers, staff and music therapists. Aging Ment Health 18: 706-716. [Crossref]
- Poli LF, Bieleninik L, Brondino N, Chen X, Gold C (2018) The effect of music therapy on cognitive functions in patients with dementia: a systematic review and meta-analysis. Aging Ment Health 22: 1097-1106. [Crossref]
- Guétin S, Portet F, Picot MC, Pommié C, Messaoudi M et al. (2009) Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: randomised, controlled study. Dement Geriatr Cogn Disord 28: 36-46. [Crossref]
- Van de Winckel A, Fey H, De Weerdt W, Dom R (2004) Cognitive and behavioral effects of music-based exercises in patients with dementia. Clin Rehabil 18: 253-260. [Crossref]
- Ying Y, Yanzhen W, Yulei S, Yamei B (2019) Meta-analysis of music therapy on intervention in patients with dementia. Chineese Nursing Res 33: 1275-1282.
- Leva V, Guy M (2013) Musical Intervention for Patients with Dementia: a meta-analysis. J Clin Nursing 22: 1203-1216.
- Watanabe K, Torikawa S, Shiota K, Matsui H, Shigenobu K et al. (2003) A study on the effects of music therapy for patients with dementia. Seishin Igaku (Clinical Psychiatry) 45: 49-54.
- Lyu J, Zhang J, Mu H, Li W, Champ M et al. (2018) The effects of music therapy on cognition, psychiatric symptoms, and activities of daily living in patients with Alzheimer’s disease. J Alzheimer's Dis 64: 1347-1358. [Crossref]
- Svansdottir H B, Snaedal J (2006) Music therapy in moderate and severe dementia of alzheimer's type: A case-control study. Int Psychogeriatrics 18: 613-621. [Crossref]
- Lin Y, Chu H, Yang C, Chen C, Chen S et al. (2011) Effectiveness of group music intervention against agitated behavior in elderly persons with dementia. Int J Geriatric Psychiatry 26: 670-678. [Crossref]
- Palisson J, Roussel-Baclet C, Maillet D, Belin C, Ankri J et al. (2015) Music enhances verbal episodic memory in alzheimer's disease. J Clin Exp Neuropsychol 37: 503-517. [Crossref]
- Lou MF (2001) The use of music to decrease agitated behaviour of the demented elderly: the state of the science. Scand J Caring Sci 15: 165-173. [Crossref]
- Choi AN, Lee M, Cheong K, Lee J (2009) Effects of Group Music Intervention on Behavioral and Psychological Symptoms in Patients with Dementia: A Pilot-Controlled Trial. Int J Neurosci 119: 471-481. [Crossref]
- Sakamoto M, Ando H, Tsutou A (2013) Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr 25: 775-784. [Crossref]
- Merriam-Webster (2019) Music.
- Pedersen SKA, Andersen N, Ricardo L, Marita A, Stefan S (2017) Effects of Music on Agitation in Dementia: A Meta-Analysis. Front Psychol 8: 742. [Crossref]
- American Music Therapy Association (2019) What is Music Therapy.
- Mayo Clinic (2019) Vascular Dementia. National Institute of Neurological Disorders.
- Stroke (NIH) (2019) Focus on Lewy Body Dementia (LBD) Research.
