A Rare Presentation of Warthin’s Tumour in the Submandibular Gland of a 7- Year-Old Boy
A B S T R A C T
A seven-year-old boy presented with a painless swelling of the right submandibular salivary gland for 1 year. The submandibular swelling was not associated with any calculus. Right submandibular sialo adenectomy done. Surprisingly the histopathology came as Warthin’s tumour. Warthin’s tumour mostly occurs in parotid gland in older age group. Because of the rare occurrence of this tumour in a young boy in extra parotid location, the case is reported.
Keywords
Salivary gland neoplasm, Warthin’s tumour, submandibular sialo adenectomy
Introduction
The salivary glands are the site of origin of a wide variety of benign and malignant neoplasm. The histopathology of these tumours are said to be the most complex and diverse of any organ in the body. About 80% of them arise from parotid, 10% from submandibular and remaining from minor salivary gland. Pleomorphic adenoma or mixed parotid tumour is the commonest tumor of the parotid and Warthin’s tumor is the second commonest. They constitute about 2% of all head and neck neoplasm. The initial description of the tumour goes back to Hildebrand in 1895, who considered this as a variant of congenital epithelial cyst of the neck. In 1910, Albreccht Arzt reported two tumours of the upper neck region which they interpreted as ‘confused tissue’ in the endodermal pharyngeal derivatives in the lymph node. They called them papillary cystadenoma of lymph nodes.
In the WHO classification of tumour, the disease was named Warthin’s tumour after the pathologist who published first two cases in American literature in 1929. He named the tumour papillary cysadenoma lymphatosum. The term Warthin’s tumour was chosen later in order to avoid confusion with malignant lymphoma[1, 2]. The great majority of these tumours occur in the lower pole of the parotid gland. Only 6-10% cases are reported outside the parotid. The extra-parotid locations are cervical lymph node, submadibular gland and larynx. These extraparotid location of these tumour has clinical significance rather than the common occurrence of the tumour in the parotid gland [3]. This is a benign tumour. Malignant transformation is rare. Local recurrence is also rare after surgical excision [4].
Case Report
A 7-year-old boy presented with a painless swelling over the right side of the neck for 1 year. The swelling was located over the right submandibular area. On examination the swelling was ovoid, non-tender, no pulsatile, the surface was smooth with soft to firm consistency. On bi-manual palpation the swelling was found to be arising from submandibular gland. No calculus was palpable. Right submandibular gland was completely excised. Lingual and hypoglossal nerves were preserved. The gland was found to be having lobulated surface (Figure 1). The tumour involved the whole gland as the gland size was increased by many folds.
Figure 1: Operative picture of the lobulated sub-mandibular gland tumor.
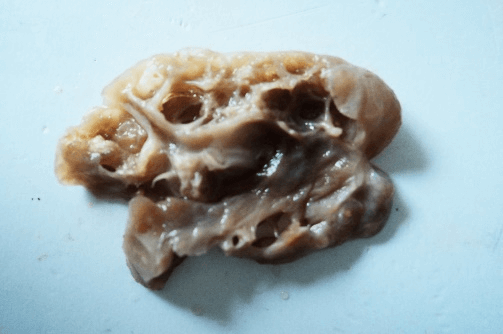
On gross pathology the gland was lobulated with thin capsule. The cut surface showed multiple cystic spaces separated by multiple septa and contained dark brown coloured fluid. (Figure 2). On microscopy the tumor had distinct two component, the epithelial and lymphoid component, which are diagnostic of Warthin’s tumour. The epithelial component consisted of multiple cystic spaces lined by double layered epithelial lining. The lymphoid component had large collection of lymphoid tissue adjacent to the epithelial tissue. (Figure 3).
Figure 2: Gross picture of the tumour showing cystic spaces.
Figure 3: Microscopic picture showing two component-epithelial and lymphoid part.
Discussion
Warthin’s tumour commonly presents as slow growing round or oval mass in the parotid gland usually at 4th to 7th decade of life [5]. These tumours mostly occur in white men. A great majority of patient have history of smoking [6]. Grossly, Warthin’s tumour possesses smooth lobulated surface and thin but tough capsule. The diagnosis is obvious just by the appearance of the cut surface of the tumour. Multiple cysts of varying diameter containing viscous dark brown “machinery fluid” are seen. The lymphoid components make up the solid area of the tumour. The pathognomonic microscopic features are epithelial cells forming papillary projections into the cystic spaces in the background of lymphoid stroma. Various theories have been put forward to explain the development of Warthin’s tumour, only two have ultimately remained. The first is the hypothesis of heterotopias.
The second is the theory that the tumour is an adenoma with lymphocytic infiltration. The first theory says that the tumour develops due to salivary gland heterotopias in periparotid and intraparotid lymph nodes. During embryogenesis of the parotid gland epithelial cells from the oral mucosa happen to penetrate the lymphoid rich tissue. Later the parotid gland gets encapsulated. According to this theory Warthin’s tumour develop in this epithelial inclusion [7]. The extraparotid locations and multicentric nature of these tumour can be explained by the last-mentioned hypothesis, where the adenoma is subsequently infiltrated by lymphocytes probably as a result of inflammatory and immune response evoked by the tumour [8].
Conclusion
Our case falls to the rare category of 6-10% extarparotid occurence of Warthin’s tumour. This case was also unique as it presented in a 7-year-old boy instead of elderly men. Gross and microscopic features were very typical of Warthin’s tumour. Authors in this field have the opinion that these extraparotid Warthin’s tumour have more research and academic importance than numerous Warthin’s tumour in the parotid gland. The reason is that the extraparotid locations can simulate lymphoma or epithelial neoplasm with secondary cystic or necrotic changes.
Article Info
Article Type
Case ReportPublication history
Received: Wed 15, Jan 2020Accepted: Wed 12, Feb 2020
Published: Mon 24, Feb 2020
Copyright
© 2023 Sardar Rezaul Islam. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ACO.2020.01.04
Author Info
Sardar Rezaul Islam Zahangir Boksh
Corresponding Author
Sardar Rezaul IslamDepartment of Surgery, Imperial Hospital, Chattogram, Bangladesh
Figures & Tables


References
- Eds Ellis GL, Auclair PL, Gnepp DR (1991) Surgical Pathology of the Salivary Glands. Philadelphia, WB Sauders.
- Eda Seifert G, Miehlke A, Haubrich J, Chilla R (1986) Diseases of the Salivary Glands. New York, Thieme Inc.
- Aguirre JM, Echebarria MA, Martinez Conde R, Rodriguez C, Burgos JJ et al. (1998) Warthin Tumor. A new hypothesis concerning its development. Oral Surg Oral Med Oral Pathol Oral radiol Endod 85: 60-63. [Crossref]
- Martins C, Fonseca I, Roque L, Soares J (1997) Cytogenetic characterisation of Warthin’s tumour. Oral Oncol 33: 344-347. [Crossref]
- Fehr A, Roser K, Belge G, Löning T, Bullerdiek J (2008) A closer look at Warthin tumors and the t(11;19). Cancer Genet Cytogenet 180: 135-139. [Crossref]
- Teymortash A, Krasnewicz Y, Werner JA (2006) Clinical features of cystadenolymphoma (Warthin's tumor) of the parotid gland: a retrospective comparative study of 96 cases. Oral Oncol 42: 569-573. [Crossref]
- Teymortash A (2008) Head and Neck: Salivary gland: Warthin’s Tumour. Atlas Genet Cytogenet Oncol Haematol.
- Eveson JW, Cawson RA (1986) Warthin's tumor (cystadenolymphoma) of salivary glands. A clinicopathologic investigation of 278 cases. Oral Surg Oral Med Oral Pathol 61: 256-262. [Crossref]
