A Rare Case of Recurrent Phyllodes Tumor of Bilateral Breasts with Metastasis to the Retroperitoneum and Duodenum
A B S T R A C T
Phyllodes tumors are uncommon fibroepithelial tumors of the breast. These tumors are graded based on the World Health Organization criteria into benign, borderline, and malignant subtypes. While benign phyllodes tumors are by far the most common presentation, borderline and malignant tumors have important clinical implications, as they are more likely to locally recur and metastasize. The most common sites of distant metastasis include the lung, bone, heart, and liver. Rare spread to the small intestines, kidney and pelvis have also been reported. We report a case of a 71-year-old woman with a history of locally recurrent phyllodes tumor of the breasts found to have retroperitoneal and intraperitoneal metastases. The retroperitoneal mass was just below the left kidney, extending into the pelvis, and overlying the psoas and iliacus muscle. The second mass involved the second portion of the duodenum, the proximal transverse colon, and the overlying mesentery. This is a rare case of delayed metastatic spread of phyllodes tumor to two sites, seventeen years after first presentation.
Keywords
Metastatic, Phyllodes, Retroperitoneum, Intraperitoneum, Duodenum
Introduction
Phyllodes tumors are rare fibroepithelial neoplasms of the breast, representing just 0.2-2% of all breast cancers [1-4]. These tumors typically present in older women as mobile, multinodular, non-painful masses, with a median age at diagnosis of 40 to 45 years-old [4, 5]. Characterized by their leaf-like appearance on microscopy, phyllodes tumors are currently graded histologically by the World Health Organization (WHO) into benign, borderline, and malignant subtypes based on specific features including the degree of stromal cellular atypia, stromal overgrowth, mitotic activity, and presence of infiltrative margins [1, 6].
The grade of phyllodes tumors has significant clinical implications as risk of local recurrence as well as hematogenous metastases increases as grade progresses from benign to borderline to malignant phyllodes tumors [7, 8]. Most phyllodes tumors behave in a benign manner. However, in the case of metastatic spread of the disease, the most commonly involved sites include the lung, bone, heart and liver [4, 9, 10]. In addition, there is a small number of reports in the literature of metastasis to the small intestine, kidney, and pelvis [9-13]. We report a case of a 71-year-old woman with history of locally recurrent phyllodes tumor of both breasts presenting with several weeks of left back pain and found to have two large metastases. This case highlights a unique location of a rare, aggressive tumor.
Case Presentation
Our patient is a 71-year-old woman with a history of hypercholesterolemia and osteoporosis who was diagnosed with a phyllodes tumor of the left breast in 2002. The breast mass was resected via lumpectomy with subsequent re-excision of positive margins. Her surgical history is also notable for laparoscopic bilateral salpingo-oophorectomy for an expanding benign tumor of the left ovary and excision of basal cell carcinoma of the skin overlying the left mid-abdominal region. She was disease-free for twelve years. In 2014, a small palpable subcutaneous nodule was noted at the left breast circumareolar scar. The mass was excised, and pathology revealed atypical spindle cell proliferation concerning for recurrent low grade phyllodes.
Three years later, in 2017, the patient developed a palpable left axillary mass with left axillary lymphadenopathy. MRI revealed a lobulated nodule in the left axilla, foci of enhancement in the lower outer quadrant of the left breast and an enhancing nodule in the right breast retro areolar region. Biopsy of the left axillary mass revealed atypical spindle cell proliferation, suspicious for metastatic phyllodes tumor to the axillary lymph nodes. Staging workup did not reveal any evidence of distant metastasis outside of the left axilla.
Left axillary lymphadenectomy and right breast lumpectomy were performed. Pathology of the axillary specimen revealed atypical spindle cell neoplasm, consistent with borderline- and intermediate-grade phyllodes tumor and twenty-nine benign lymph nodes. It was difficult to determine whether this single mass represented a separate parenchymal phyllodes tumor or lymph node metastasis with complete architectural obliteration. Supporting the diagnosis of phyllodes tumor, immunohistochemical stains were negative for CK5/6, HWMCK, p63 and myogenin. Right breast lumpectomy pathology showed probable but not definitive diagnosis of benign phyllodes tumor. This diagnosis was based on the presence of a benign spindle cell lesion with surrounding fat necrosis.
Figures 1: Coronal view of left retroperitoneal and paraduodenal mass.
Horizontal arrow pointing to the left retroperitoneal mass extending from below the inferior pole of the left kidney into the pelvis. Vertical arrow pointing to the mass involving the second portion of the duodenum extending to the hepatic flexure.
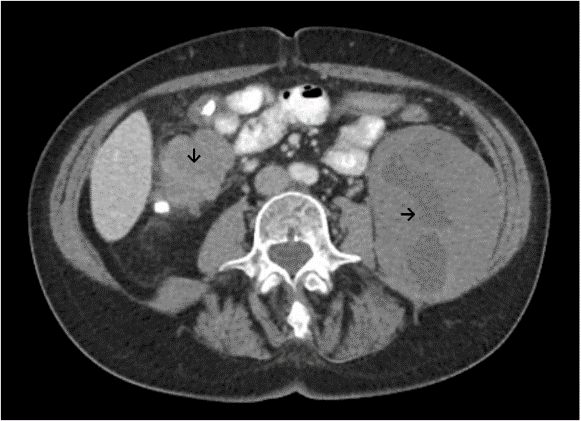
The patient presented again in 2019 with complaint of left back pain, loss of appetite and weight loss of ten pounds. She did not have lower extremity neuropathy, sensory or motor loss and did not experience nausea, vomiting, hematemesis or hematochezia. MRI revealed a left retroperitoneal mass approximately 8cm x 8cm in size, extending from below the inferior pole of the left kidney into the pelvis (Figures 1 & 2; horizontal arrow). A 4cm x 5cm mass was noted involving the second portion of the duodenum extending to the hepatic flexure (Figures 1 & 2; vertical arrow). The abdomen was soft, nontender and nondistended without evidence of any palpable masses or ascites. The patient had endoscopic ultrasound-guided biopsies of the masses which were consistent with metastatic phyllodes tumor similar to the left breast lesion excised in 2002. Imaging did not reveal evidence of disease outside the abdomen. Given the patient’s presentation of debilitating back pain, surgical resection was planned.
Figures 2: Transverse view of left retroperitoneal and paraduodenal mass. Horizontal arrow pointing to the left retroperitoneal mass extending from below the inferior pole of the left kidney into the pelvis. Vertical arrow pointing to the mass involving the second portion of the duodenum extending to the hepatic flexure.
The patient underwent an exploratory laparotomy with radical resection of the left retroperitoneal mass located below the inferior pole of the left kidney, sitting on the psoas and iliacus muscles, and extending into the pelvis. The mass was removed en bloc with grossly clear margins. The second mass in the right upper quadrant was mobile but found to be involving the anterior and lateral wall of the second portion of the duodenum as well as the mesentery and serosal layer of proximal transverse colon. In order to achieve clear margins, a right hemicolectomy with ileocolic anastomosis, partial duodenal resection with primary closure, and omental flap over the duodenal repair was performed. A right hemicolectomy with ileocolic anastomosis was done instead of a segmental transverse colectomy with colo-colonic anastomosis in order to minimize risk of postoperative bowel leak.
Postoperative course was unremarkable and upper GI series on postoperative day (POD) four showed no evidence of duodenal leak. The patient’s diet was advanced after return of bowel function, and she was discharged home on POD six without any complications. Pathology of the retroperitoneal mass and the right upper quadrant mass showed spindle cell neoplasm consistent with metastatic malignant phyllodes tumor in the abdomen.
Discussion
Phyllodes tumors of the breast make up a small portion of all breast cancers, with roughly 500 women in the United States diagnosed each year [4]. Phyllodes tumors represent a spectrum of disease, ranging from benign to borderline to malignant grade tumors. Benign phyllodes tumors make up 60 to 75% of cases and resemble fibroadenomas of the breast. More closely resembling sarcomas, malignant tumors (10-20% of cases) are characterized histologically by marked stromal cellularity and atypia, high mitotic activity (>10 per 10 HPF), stromal overgrowth, and infiltrative tumor borders [4, 14]. Distinguishing between borderline and malignant tumors is sometimes difficult to make due to their overlapping pathologic features, but overall a borderline designation (13-26% of cases) is assigned to tumors of an intermediate presentation [7, 14].
The histologic grade of phyllodes tumors guides clinical prognosis as borderline and malignant tumors are much more likely to locally recur or metastasize [8]. The poor pathologic features of malignant tumors are associated with worse clinical outcomes, including a 66% ten-year survival compared to a 100% ten-year survival of patients without poor features [15]. A recent review of the literature found pooled local recurrence rates for benign, borderline, and malignant tumors to be 8%, 13%, and 18%, respectively [8]. Moreover, local recurrence of a phyllodes tumor serves as one risk factor for metastatic disease [16]. Tumor metastasis typically occurs within the initial two years of diagnosis, and tumors of a malignant grade have the highest rates of distant metastasis (22-40) % [4, 9, 17]. Metastatic phyllodes tumors are known to spread hematogenously, with the most common sites of metastasis including the lung (66%-84.5%), bone (28%-39%), brain and liver [4, 9, 10, 12]. Unusual sites for distant metastases have also been described in the literature, including the adrenal gland, small intestine, kidney, pancreas, and pelvis [9-13].
Our patient presented with rare sites of metastasis of phyllodes tumor into the retroperitoneal and intraperitoneal spaces, including involvement of the proximal transverse colon, mesentery, and duodenum. There is a limited number of reported cases of phyllodes tumors involving the gastrointestinal tract. To our knowledge, there are two case reports in the literature, one of a gastrointestinal bleed due to tumor involvement of the duodenum and another case of small bowel obstruction related to tumor metastases to the ileum [9, 11].
Moreover, our patient had tumor involvement in the retroperitoneum, from below the kidney into the pelvic cavity. One other case report has described similar tumor involvement of the pelvis [13]. Of note, our patient did not have any metastatic involvement of the lungs, the most common area of involvement for metastatic phyllodes tumors. While most metastatic disease occurs in the first two years of diagnosis, there have been other reported cases of a delayed rather than synchronous presentation of up to thirteen years after diagnosis [10, 18]. Our patient presented with metastatic disease seventeen years after her initial diagnosis.
Finally, the patient’s tumor progressed from borderline grade at initial presentation to malignant grade at the sites of distant metastases. This worsening of pathologic features with local recurrence of disease has been previously described in the literature [8]. While locally recurrent tumors most often present as the same grade as the original tumor, one systematic review of 54 retrospective studies found 26% of benign and 21% of borderline tumors locally recur at a higher grade (borderline or malignant) [8].
For the treatment of phyllodes tumors, the National Comprehensive Cancer Network (NCCN) guidelines recommend wide excision with one-centimeter margin, without axillary lymph node dissection [3, 4, 15, 19]. There are currently no randomized controlled trials studying the efficacy of adjuvant radiation therapy on these tumors. However, the NCCN guidelines recommend consideration of adjuvant radiation, especially in the treatment of borderline and malignant tumors [1, 3, 4, 19, 20]. Currently, the efficacy of chemotherapy as treatment for phyllodes tumors has not been well shown in the literature. Mitus et al. (2016) found doxorubicin and ifosfamide-based chemotherapies to have some efficacy in the treatment of metastatic disease, but more literature is needed to determine a role for chemotherapy in the treatment of phyllodes tumors [21]. Based on current guidelines, the patient in this case may have benefitted from adjuvant radiation therapy on her initial presentation or during her first local recurrence. Ultimately, the prognosis for patients with distant metastases is very poor, with few patients surviving a year after diagnosis [10]. For borderline and malignant phyllodes tumors, the importance of negative margins is paramount, as excess surgical margins have been shown to be a risk factor for local recurrence as well as distant metastasis [20]. Therefore, complete tumor excision with mastectomy, if needed, should be considered [20].
This case presents an unusual instance of metastatic spread of a phyllodes tumor seventeen years after initial diagnosis, as well as a rare site of metastasis in the retroperitoneal and intraperitoneal spaces, without metastatic spread to the lungs. This case highlights the need for clear guidelines for the use of adjuvant radiation therapy in the initial treatment of or in the management of local recurrence for borderline and malignant phyllodes tumors. Metastatic malignant phyllodes tumors represent a group of aggressive neoplasms where complete surgical excision with wide margins and proper follow-up are vital to treatment of the disease.
Disclosure
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 27, Mar 2020Accepted: Wed 15, Apr 2020
Published: Wed 29, Apr 2020
Copyright
© 2023 Poya Pourghaderi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2020.01.05
Author Info
Andrew M. Nouri Poya Pourghaderi Sara E. Chapin Zoltan Nemeth Zubin M. Bamboat
Corresponding Author
Poya PourghaderiDepartment of Surgery, Morristown Medical Center, Morristown, New Jersey, USA
Figures & Tables
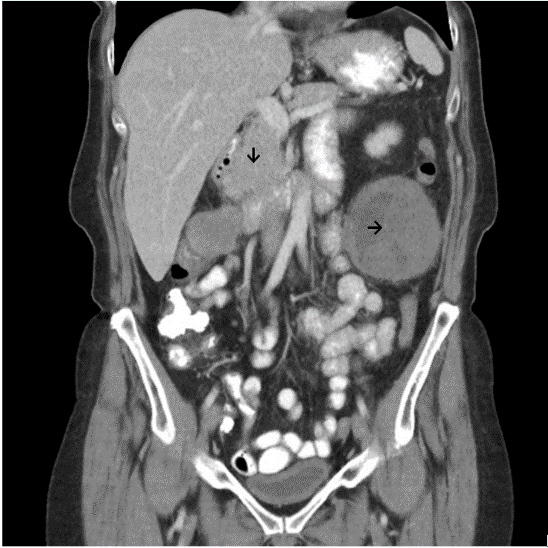
Horizontal arrow pointing to the left retroperitoneal mass extending from below the inferior pole of the left kidney into the pelvis. Vertical arrow pointing to the mass involving the second portion of the duodenum extending to the hepatic flexure.
References
- Mitus JW, Blecharz P, Jakubowicz J, Reinfuss M, Walasek T et al. (2019) Phyllodes tumors of the breast. The treatment results for 340 patients from a single cancer centre. Breast 43: 85-90. [Crossref]
- Vorherr H, Vorherr UF, Kutvirt DM, Key CR (1985) Cystosarcoma phyllodes: epidemiology, pathohistology, pathobiology, diagnosis, therapy, and survival. Arch Gynecol 236: 173-181. [Crossref]
- Belkacémi Y, Bousquet G, Marsiglia H, Ray Coquard I, Magné N et al. (2008) Phyllodes tumor of the breast. Int J Radiat Oncol Biol Phys 70: 492-500. [Crossref]
- Strode M, Khoury T, Mangieri C, Takabe K (2017) Update on the diagnosis and management of malignant phyllodes tumors of the breast. Breast 33: 91-96. [Crossref]
- Khosravi Shahi P (2011) Management of non-metastatic phyllodes tumors of the breast: review of the literature. Surg Oncol 20: e143-e148. [Crossref]
- Zhang Y, Kleer CG (2016) Phyllodes tumor of the breast: Histopathologic Features, Differential Diagnosis, and Molecular/ Genetic Updates. Arch Pathol Lab Med 140: 665-671. [Crossref]
- Tan BY, Acs G, Apple SK, Badve S, Bleiweiss IJ et al. (2016) Phyllodes tumours of the breast: a consensus review. Histopathology 68: 5-21. [Crossref]
- Lu Y, Chen Y, Zhu L, Cartwright P, Song E et al. (2019) Local Recurrence of Benign, Borderline, and Malignant Phyllodes Tumors of the Breast: A Systematic Review and Meta-analysis. Ann Surg Oncol 26: 1263-1275. [Crossref]
- Asoglu O, Karanlik H, Barbaros U, Yanar H, Kapran Y et al. (2006) Malignant phyllode tumor metastatic to the duodenum. World J Gastroenterol 12: 1649-1651. [Crossref]
- Ramakant P, Selvamani, Therese MM, Paul MJ (2015) Metastatic Malignant Phyllodes Tumor of the Breast: An Aggressive Disease-Analysis of 7 Cases. Indian J Surg Oncol 6: 363-369. [Crossref]
- Kelly RJ, Barrett C, Swan N, McDermott R (2009) Metastatic phyllodes tumor causing small-bowel obstruction. Clin Breast Cancer 9: 193-195. [Crossref]
- Karczmarek Borowska B, Bukala A, Syrek Kaplita K, Ksiazek M, Filipowska J et al. (2015) A Rare Case of Breast Malignant Phyllodes Tumor With Metastases to the Kidney: Case Report. Medicine (Baltimore) 94: e1312. [Crossref]
- Shan J, Zhang S, Wang Z, Fu Y, Li L et al. (2016) Breast malignant phyllodes tumor with rare pelvic metastases and long-term overall survival: A case report and literature review. Medicine (Baltimore) 95: e4942. [Crossref]
- Wang Y, Zhang Y, Chen G, Liu F, Liu C et al. (2018) Huge borderline phyllodes breast tumor with repeated recurrences and progression toward more malignant phenotype: a case report and literature review. Onco Targets Ther 11: 7787-7793. [Crossref]
- Spanheimer PM, Murray MP, Zabor EC, Stempel M, Morrow M et al. (2019) Long-Term Outcomes After Surgical Treatment of Malignant/Borderline Phyllodes Tumors of the Breast. Ann Surg Oncol 6: 2136-2143. [Crossref]
- Wei J, Tan YT, Cai YC, Yuan ZY, Yang D et al. (2014) Predictive factors for the local recurrence and distant metastasis of phyllodes tumors of the breast: a retrospective analysis of 192 cases at a single center. Chin J Cancer 33: 492-500. [Crossref]
- Pimiento JM, Gadgil PV, Santillan AA, Lee MC, Esposito NN et al. (2011) Phyllodes tumors: race-related differences. J Am Coll Surg 213: 537-542. [Crossref]
- Amir RA, Rabah RS, Sheikh SS (2018) Malignant Phyllodes Tumor of the Breast with Metastasis to the Pancreas: A Case Report and Review of Literature. Case Rep Oncol Med 2018: 6491675. [Crossref]
- Adesoye T, Neuman HB, Wilke LG, Schumacher JR, Steiman J et al. (2016) Current Trends in the Management of Phyllodes Tumors of the Breast. Ann Surg Oncol 23: 3199-3205. [Crossref]
- Kapiris I, Nasiri N, A'Hern R, Healy V, Gui GP (2001) Outcome and predictive factors of local recurrence and distant metastases following primary surgical treatment of high-grade malignant phyllodes tumours of the breast. Eur J Surg Oncol 27: 723-730. [Crossref]
- Mituś JW, Blecharz P, Walasek T, Reinfuss M, Jakubowicz J et al. (2016) Treatment of Patients with Distant Metastases from Phyllodes Tumor of the Breast. World J Surg 40: 323-328. [Crossref]
