A Rapidly Fatal Case of Lactobacillus Rhamnosus Sepsis Associated with Thyroid Storm in an Immunocompetent Patient
A B S T R A C T
We report a rapidly fatal case of 29-year-old man who presented with typical features of sepsis along with thyrotoxicosis. Presence of thrombotic lesions in his lower extremities led to the assumption that the source of infection could be endocarditis. However, transthoracic echocardiography did not confirm the preliminary diagnosis. Report of facultative anaerobic Gram-positive bacilli seen in the Gram stain of positive blood culture prompted initiation of treatment with ceftriaxone, vancomycin and metronidazole. Thyrotoxicosis was managed with propranolol, propylthiouracil, Lugol’s iodine and hydrocortisone. Diagnostic criteria for thyroid storm and infective endocarditis and therapy of Lactobacillus sepsis with a possible cause of death in the present case are discussed.
Keywords
L. rhamnosus, bacteremia, thyrotoxicosis, thyroid storm, sepsis, management
Introduction
Thyroid storm, also referred to as thyrotoxic crisis, is an acute, life-threatening, hypermetabolic state observed in individuals with thyrotoxicosis [1]. The overall incidence of hyperthyroidism is estimated to be around 1%, with the majority of cases being subclinical in terms of presentation [2]. Among hospitalized hyperthyroid patients, the incidence of thyroid storm has been noted to be <10% [2, 3]. However, the mortality rate of thyroid storm without treatment is about 90%, which drops to about 30% with treatment [2]. Patients may suffer from congestive heart failure, sepsis, or respiratory failure ultimately leading to death due to multiple organ failure (MOF) [2-5].
Lactobacillus spp. are ubiquitous commensals of normal human flora in the oral cavity, gastrointestinal tract and female genital tract and have only occasionally been associated with serious infections [6, 7]. Lactobacillus bacteremia is an uncommon entity that usually occurs in patients with severe underlying conditions, which include cancer, organ transplantation, diabetes mellitus and recent surgery [8]. More often than not Lactobacillus bacteremia is seen in patients with infective endocarditis with an earlier report implicating it as a causative agent in 0.05-0.4% of all endocarditis [9, 10].
We present a patient of thyrotoxicosis who turned a fulminate course and succumbed to MOF as a result of complication of Lactobacillus rhamnosus sepsis. This case report discusses the factors leading to diagnostic delay and highlights the dangerous manifestations of sepsis in a thyrotoxic patient. While infection is a known precipitant of thyroid storm, this report reflects, to the authors’ best knowledge, the first depiction of sepsis due to L. rhamnosus infection apparently precipitating thyroid storm.
Case Report
A 29-year-old man was brought to the emergency room of Farwaniya Hospital in Kuwait. The medical history revealed that the patient had been suffering from palpitation for 5 days and left second toe pain for 2 days. He did not give history of shortness of breath, chest pain, double vision, change of bowel habit or urinary symptoms. The past or family history was unremarkable. On examination the patient appeared conscious, alert but in respiratory distress. His physical examination revealed the pulse rate to be 138/min., temperature 39.3oC(102.7oF), blood pressure 120/72 mm Hg, respiratory rate 30/min, SPO2 98%, exophthalmos, clubbing of fingernails, soft and lax abdomen with no organomegaly or tenderness and a S1S2 pansystolic murmur. The left leg was found to be grossly intact although no peripheral pulses were palpable below the popliteal artery. A blackish spot was observed on left second toe while no abnormality was noticed in the right lower extremity. Also, a diffuse bilateral swelling was apparent in front of the neck, which was non-tender on palpation and appeared to be associated with the thyroid gland (goiter). No enlarged lymph nodes were felt in the neck or other parts of the body.
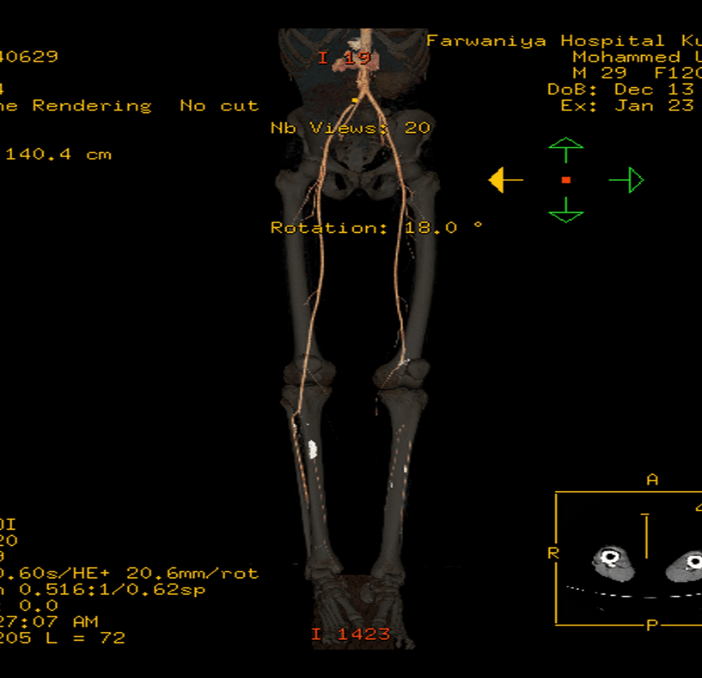
Laboratory investigations: At the time of admission the laboratory tests showed WBC count 13.1x109/L; hemoglobin 118 g/L; INR 1.32; fibrinogen 5.2 g/L; TSH <0.005 µIU/mL; T4 58.04 pmol/L; ALT 19 IU/L; AST 22 IU/L; creatinine 45 µmol/L ; troponin I 0.06 µg/L and glucose 6.28 mmol/L. However, after 48 h WBC had risen to 46.6 x 109/L with 90.9% neutrophils, procalcitonin 0.513 ng/L; CRP 54.0 mg/L; INR 9.7; fibrinogen 2.2 g/L; ALT 3859 IU/L; AST 9947 IU/L; urea 18.5 mmol/L; creatinine 233.0 mmol/L; troponin I 31.04 µg/L and glucose 12.1 mmol/L. Radiological assessment: Computed tomography angiography of the arterial tree of the lower limbs demonstrated adequate opacification of most of the vessels except genicular and infragenicular portion of the popliteal artery as well as proximal tiboperioneal trunk of the left leg (Figure 1). Alternating stenosis and thrombosis of the infragenicular arteries bilaterally indicated peripheral vascular disease. Bedside transthoracic electrocardiography (TTE) revealed flail anterior mitral valve leaflet with severe mitral regurgitation, ruptured chordae tendinae and dilated left atrium with compensated (>60%) left ventricular function. However, no vegetations were seen.
Figure 1: CT angiogram of both lower limbs showing complete occlusion of left popliteal artery just above the knee and the vessel is occluded below the knee on the right side.
Microbiology: Blood sample collected for culture (BACTEC FX, Becton Dickinson & Co., USA) from two separate venepuncture sites yielded growth of Gram-positive rods in three bottles (two anaerobic and one aerobic bottle) of two sets (four bottles) collected on admission. After 48 h the isolate was identified as L. rhamnosus by Phoenix (Becton Dickinson & Co., USA) and confirmed by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF/MS) Vitek MS (Biomerieux, France) with accuracy of 93.4%. Antimicrobial susceptibility testing (AST) was performed by disk diffusion method (Oxoid, Basingstoke, UK) on Mueller-Hinton agar with 5% sheep blood and interpreted according to the published guidelines [11, 12]. The organism was found to be susceptible to ampicillin, cefuroxime, cefotaxime, clindamycin, erythromycin, piperacillin/tazobactam and resistant to metronidazole and vancomycin.
Management: Empirical therapy with ceftriaxone plus vancomycin was initiated at the time of presentation. However, following the Gram stain report of the blood culture sample metronidazole was added by the treating physician. As a treatment for hyperthyroidism the patient received propylthiouracil, propranolol, Lugol’s iodine and hydrocortisone following the recommended guidelines [13]. Unfortunately, the patient died of MOF on the medical ward in less than 72 h of presenting in the emergency room.
Discussion
Lactobacilli are Gram-positive, non-motile, non-spore-forming, and microaerophilic, which are usually catalase-negative and require complex nutrients for optimum growth. Identifying the organism can be challenging in a general hospital diagnostic laboratory. In a previous report Lactobacillus spp. were identified by 16S rRNA sequencing analysis and MALDI-TOF/MS. While MALDI-TOF/MS provided correct identification for 84.9% (73/86) of Lactobacillus isolates concordant identification was lowest for L. casei (11%) [14]. In the current practice, identification of clinically relevant Gram-positive organisms can be optimized by use of MALDI-TOF/MS as evidenced in yet another study [15]. Data regarding antimicrobial susceptibility of clinical Lactobacillus spp. isolates are scarce, and appropriate interpretation criteria for susceptibility tests are not available. In an earlier study, data on AST performed by disk diffusion method the strain of L. rhamnosus was reported to be resistant to cefotaxime unlike our strain [16]. Data reported for 46 isolates of L. rhamnosus demonstrated low minimum inhibitory concentrations (MICs) of imipenem, piperacillin-tazobactam, erythromycin, and clindamycin. MICs of vancomycin were high (>256 µg/mL) [17]. In the report by Lee et al. (2015) AST was performed by broth dilution method and MICs were found to be highest for glycopeptides, cephalosporins and fluoroquinolones and lowest for carbapenems and aminopenicillins. Generally, several bacterial species in the genus Lactobacillus, which form part of the normal human microbiota, are considered nonpathogenic and isolation of these organisms from blood samples is dismissed as contamination. In a previous retrospective study, relationship between Lactobacillus spp. and the site from which the species was recovered was studied [18]. Of 19 blood culture isolates (17.7% of all lactobacilli isolated from different sites), seven (29%) were identified as L. rhamnosus. Of 10 clinically significant cases of bacteremia due to Lactobacillus spp., L. rhamnosus (60%) was the most common species, which was found to be associated with an underlying disease such as esophageal carcinoma, pancreatitis, HIV, Crohn’s disease etc. Interestingly, none of these patients was associated with infective endocarditis [18]. Lactobacillus bacteremia is a rare entity, and its clinical significance in immuno-competent patients is poorly defined [19]. However, since the organism was grown in three of four blood culture bottles, it illustrated unequivocally the isolate to be a pathogen in our patient. In this context, accurate identification of the Lactobacillus spp. has been questioned in studies reported in the past affecting the interpretation of their clinical significance because a reliable molecular method such as 16S rRNA gene sequence analysis became commonly accessible only after 2005 [19]. Previous frequent association of lactobacilli with endocarditis is explained by misidentification of isolates as suggested by most strains being reported as susceptible to vancomycin [20]. In view of the peripheral vascular disease with thrombotic lesions in the lower extremity in our patient there was a strong suspicion of infective endocarditis. Inconclusive result of TTE prompted the decision to confirm the diagnosis by transesophageal electrocardiography, which however was not possible because of the rapid deterioration of the patient’s general condition. Despite bacteremia, temperature > 380C, predisposing heart condition and embolic phenomenon in our patient diagnosis of infective endocarditis was not possible based on modified Duke criteria [21]. We, however, feel encouraged to believe that the patient would have probably emerged as a case of infective endocarditis, had all the relevant investigations been completed. In a previous study, the patients with L. rhamnosus bacteremia had severe or fatal comorbidities and in multivariate analysis it was determined that severe underlying diseases were a significant predictor for mortality (odds ratio,OR, 15.8); however, treatment with antimicrobials effective in vitro was associated with lower mortality (OR, 0.22) [19].
The patient's symptoms of fever, tachycardia, and vascular disease along with his abnormal thyroid function tests are also commonly seen in thyroid storm, which further confounded the diagnosis. Using the clinical decision rules suggested by Burch and Wartofsky, the patient would have scored 50 points (20 for tachycardia at 138 bpm, 20 for temperature at 39.3°C and 10 for precipitating event of L. rhamnosus sepsis), which is suggestive of thyroid storm (> 45 points) [3]. Thyroid storm is an extreme form of hyperthyroidism with a more severe presentation that is associated with a high mortality rate. However, it is rare and remains potentially a life-threatening medical emergency. A case of thyroid storm associated with sepsis caused by pneumonia, which had a catastrophic course including recurrent cardiac arrest and subsequent MOF was reported last year [22]. The incidence of MOF in thyroid storm has been reported to be 9% and considered to be an independent risk factor for mortality [2]. Both bacterial and viral infections are known to precipitate the occurrence of thyroid storm [3].
Exogenous sources of lactobacilli include fermented food products such as yogurt and cheeses as well as probiotics. One of the important ingredients contained in the commercially available probiotics has been found to be members of the genus Lactobacillus, which have been claimed to have beneficial effects in a variety of disorders. Studies have been undertaken to determine the pathogenic association of lactobacilli with the disease in both previously healthy individuals and patients with various underlying diseases who consumed probiotics [23]. In cases of sepsis or bacteremia caused by lactobacilli, mechanisms like bacterial translocation from the gut or other alterations in the integrity of mucosal surfaces permitting passage of microbes in the bloodstream have been hypothesized [23]. In a series of 89 episodes of bacteremia caused by lactobacilli, the majority of patients had severe underlying diseases, with a predominance of gastrointestinal or hepatic neoplasia, and a high mortality rate of 69%. In this series, L. rhamnosus was the most frequent isolate (53%); however, with no cases of endocarditis identified [19]. In a study of 73 endocarditis patients caused by lactobacilli, 63% of patients had an underlying structural heart disease. Whereas dental procedures were reported in 47% of cases, only 3 cases reported consumption of probiotics [24]. Considering the social background of our patient, it was highly unlikely that he consumed a probiotic, which contributed to sepsis in his case. We were unable to determine the source of L. rhamnosus in our patient.
It is challenging to manage these patients although successful treatment with continuous veno-venous renal replacement therapy (CRRT) with intravenous albumin and plasma supplementation in addition to reduced dose of beta-blocker and antithyroid drug has been reported [25]. Unfortunately, the management of our patient did not prove successful for the following possible reasons:
1. diagnostic dilemma with emphasis to treat hyperthyroidism,
2. initial microbiological report of Gram-positive rods in the blood culture led to initiation of treatment with ceftriaxone, metronidazole and vancomycin when the organism is inherently resistant to vancomycin and metronidazole [16]. In a study where 83% of patients with L. rhamnosus bacteremia were treated with combination therapy, mortality at 1 week was 12% among patients who presumably were receiving adequate treatment and 27% among patients who were receiving inadequate treatment (p=.131, by E-test) [17].
3. CRRT was not initiated, and
4. continued use of propranolol, which has been shown to cause cardio-respiratory arrest in such cases [25]. The cause of thrombotic lesions in lower extremity vasculature remained unexplained at the time of death. Final diagnosis in our patient remained evasive and the cause of death could not be definitely ascertained as performing autopsy on the deceased is not permissible by law in Kuwait except under special medico-legal circumstances.
Lessons learned
1. Although isolation of Lactobacillus spp. in blood cultures is often overlooked as contamination, it is suggested that in the right clinical setting Lactobacillus spp. bacteremia is a harbinger for a serious underlying pathology and should not be ignored.
2. Reports on appropriate antimicrobial agents with proven action against Lactobacillus spp. have been variable for many reasons, including methodology used for AST.
3. In patients with underlying hyperthyroidism, sepsis may mimic thyroid storm in presentation and laboratory analysis, so clinical decision making tools may be misleading.
4. Management of thyroid storm patients in the intensive care is mandatory for organ-specific revival.
Conclusion
Development of thyroid storm in a patient with thyrotoxicosis is a relatively uncommon albeit a dangerous situation. The clinical features of thyroid storm may be related to other co-morbidities which makes diagnosis a clinical challenge. In addition, patients, if diagnosed with a thyroid storm, should be treated immediately with appropriate medications. Physicians must maintain a high index of suspicion of this rare presentation as this disease can be life-threatening! L. rhamnosus sepsis can trigger onset of thyroid storm in a patient with hyperthyroidism.
Disclosure
Authors declare no conflict of interest.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 24, Sep 2019Accepted: Tue 08, Oct 2019
Published: Mon 21, Oct 2019
Copyright
© 2023 Wadha A. Alfouzan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.EJGM.2019.01.02
Author Info
Nasser Al-Rubai’aan Rita Dhar Wadha A. Alfouzan
Corresponding Author
Wadha A. AlfouzanDepartment of Laboratory Medicine, Microbiology Unit, Farwaniya Hospital, Kuwait
Figures & Tables
References
- Chiha M, Samarasinghe S, Kabaker AS (2015) Thyroid storm: an updated review. J Intensive Care Med 30: 131-140. [Crossref]
- Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S et al. (2012) Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 22: 661-679. [Crossref]
- Aslan IR, Baca EA, Charlton RW, Rosenthal SM (2011) Respiratory syncytial virus infection as a precipitant of thyroid storm in a previously undiagnosed case of graves' disease in a prepubertal girl. Int J Pediatr Endocrinol 2011: 138903. [Crossref]
- Shah SR, Millan T, Alamzaib SM, Luu SW (2018) Idiopathic thyroid storm mimicking SIRS in a patient with hypothyroidism- a diagnostic dilemma. J Community Hosp Intern Med Perspect 8: 368-369. [Crossref]
- Rayner SG, Hosseini F, Adedipe AA (2013) Sepsis mimicking thyroid storm in a patient with methimazole-induced agranulocytosis. BMJ Case Rep 2013. [Crossref]
- Gouriet F, Million M, Henri M, Fournier PE, Raoult D (2012) Lactobacillus rhamnosus bacteremia: an emerging clinical entity. Eur J ClinMicrobiol Infect Dis 31: 2469-2480. [Crossref]
- Kulkarni HS, Khoury CC (2014) Sepsis associated with Lactobacillus bacteremia in a patient with ischemic colitis. Indian J Crit Care Med 18: 606-608. [Crossref]
- Antony SJ, Stratton CW, Dummer JS (1996) Lactobacillus bacteremia: description of the clinical course in adult patients without endocarditis. Clin Infect Dis 23: 773-778. [Crossref]
- Borriello SP, Hammes WP, Holzapfel W, Marteau P, Schrezenmeir J et al. (2003) Safety of probiotics that contain lactobacilli or bifidobacteria. Clin Infect Dis 36: 775-780. [Crossref]
- Naqvi SSB, Nagendra V, Hofmeyr A (2018) Probiotic related Lactobacillus rhamnosus endocarditis in a patient with liver cirrhosis. IDCases 13: e00439. [Crossref]
- Comité de l'Antibiogramme de la SociétéFrançaise de Microbiologie (2009) Communiqué 2009. Comité de l'Antibiogramme de la Société Française de Microbiologie, Paris, France.
- Felton A, Barreau C, Bizet C, Lagrange PH, Philippon A (1999) Lactobacillus species identification, H2O2 production, and antibiotic resistance and correlation with human clinical status. J Clin Microbiol 37: 729-733. [Crossref]
- Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi Tet al. (2016) 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr J 63: 1025-1064. [Crossref]
- Lee MR, Tsai CJ, Liang SK, Lin CK, Huang YT et al. (2015) Clinical characteristics of bacteraemia caused by Lactobacillus spp. and antimicrobial susceptibilities of the isolates at a medical centre in Taiwan, 2000-2014. Int J Antimicrob Agents 46: 439-445. [Crossref]
- Fosch SE, Ficoseco CA, Marchesi A, Cocucci S, Nader-Macias MEF et al. (2018) Contraception: Influence on vaginal microbiota and identification of vaginal lactobacilli using MALDI-TOF MS and 16S rDNA sequencing. Open Microbiol J 12: 218-229. [Crossref]
- Robin F, Paillard C, Marchandin H, Demeocq F, Bonnet R et al. (2010) Lactobacillus rhamnosus meningitis following recurrent episodes of bacteremia in a child undergoing allogeneic hematopoietic stem cell transplantation. J Clin Microbiol 48: 4317-4319. [Crossref]
- Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M et al. (2006) Lactobacillus bacteremia, species identification, and antimicrobial susceptibility of 85 blood isolates. Clin Infect Dis 42: e35-e44. [Crossref]
- Martinez RM, Hulten KG, Bui U, Clarridge JE III (2014) Molecular analysis and clinical significance of Lactobacillus spp. recovered from clinical specimens presumptively associated with disease. J ClinMicrobiol 52: 30-36. [Crossref]
- Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M et al. (2004) Lactobacillus bacteremia, clinical significance, and patient outcome, with special focus on probiotic L. Rhamnosus GG. Clin Infect Di 38: 62-69. [Crossref]
- Wallet F, Dessein R, Armand S, Courcol RJ (2002) Molecular diagnosis of endocarditis due to Lactobacillus casei subsp. rhamnosus. Clin Infect Dis 35: e117-e119. [Crossref]
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr et al. (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30: 633-638. [Crossref]
- Park HS, Kwon SK, Kim YN (2017) Successful treatment of thyroid storm presenting as recurrent cardiac arrest and subsequent multiorgan failure by continuous renal replacement therapy. Endocrinol Diabetes Metab Case Rep 2017. [Crossref]
- Boumis E, Capone A, Galati V, Venditti C, Petrosillo N (2018) Probiotics and infective endocarditis in patients with hereditary hemorrhagic telangiectasia: a clinical case and a review of the literature. BMC Infect Dis 18: 65. [Crossref]
- Cannon JP, Lee TA, Bolanos JT, Danziger LH (2005) Pathogenic relevance of lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis 24: 31-40. [Crossref]
- Dalan R, Leow MK (2007) Cardiovascular collapse associated with beta blockade in thyroid storm. Exp Clin Endocrinol Diabetes 115: 392-396. [Crossref]
