Journals
A Randomized Trial of Live versus Video Delivery of Pain Neuroscience Education for Middle School Children
A B S T R A C T
Objectives:To compare if a video-delivered pain neuroscience education (PNE) session yield comparable results to a live-PNE session delivered to middle school students in terms of pain knowledge and attitudes and beliefs regarding pain. Methods:Two hundred and fifty-one 5th through 8th grade middle school students were randomly assigned to receive a live (n = 147) or video-delivered (n = 104) presentation (30 minutes). Prior to and immediately following the lectures, students completed a knowledge of pain questionnaire (Neurophysiology of Pain Questionnaire - NPQ) and beliefs regarding pain questionnaire (Health Care Provider#39;s Pain and Impairment Relationship Scale - HC-PAIRS). Results:Both video (p < 0.001) and live presentations (p < 0.001) yielded significant increases in pain knowledge and both showed large effect sizes (video 0.81 and live 0.82) as well. Pain beliefs questions of "You can control how much pain you feel" and "Your brain decides if you feel pain, not your tissues" both had significant changes (both groups p < 0.001), with moderate effect size for both groups (video .45 and .56; live .51 and 68). Conclusion:A 30-minute video-delivered PNE resulted in similar changes to a live, in-person PNE session. The results from this study may help PNE approaches for middle schools to become standardized, cost-effective and scalable. Larger trials with long-term follow-up are needed to determine if video-delivery PNE is effective in altering behavior change.
Keywords
Pain,epidemic,education,school,attitudes,beliefs
Introduction
Pain affects human beings of all races, socioeconomic backgrounds and ages [1]. Up to 25% of individuals under the age of 19 have experienced pain in the last three months, with "intense and frequent" pain being reported in 6-8% of all children [1, 2]. Furthermore, 92.5% of middle school students reported knowing someone living with persistent pain [3].
Opioid medications are frequently prescribed for those experiencing pain [4]. Adolescents experiencing acute or post-surgical pain are often exposed to opioids during medical provider visits for trauma (36.5%), dental visits (15.7%), and visits related to procedures (13.2%) [5]. This implies that children are at risk of opioid use disorder and addiction. In fact, Groenewald and Palermo found that opioid prescription in adolescence was independently associated with a 33% increased risk for opioid misuse between 19 and 23 years of age [5]. A recent study showed 27% of adolescents receiving prescriptions for opioids following surgery had prescription durations of greater than 10 days [6]. Recently the food and drug administration (FDA) published guidelines for dosing of extended release oxycodone for children as young as eleven years old [7]. The need for effective treatment of pediatric pain is self-evident: children in pain can become adults in pain, risking a staggering emotional, economic and societal burden [3, 8, 9]. These adolescent and child statistics pertaining to pain and opioid exposure/use are part of the current pain and opioid epidemic in the United States (US) and globally [10].
Throughout the history of mankind, whenever faced with epidemics, i.e., tobacco use (smoking), human immunodeficiency virus (HIV), etc., mass education has been utilized as a means to mobilize society. One non-pharmacological intervention addressing pain and the opioid epidemic that is gaining interest and holds potential to curb the rise in chronic pain and disability, as well as opioid use in adolescents, is pain neuroscience education (PNE) [3]. In people with musculoskeletal pain it has been demonstrated that educational strategies focused on the neurophysiology and neurobiology of pain (PNE) have strong evidence for improving pain ratings, pain knowledge, disability, pain catastrophization, fear-avoidance, attitudes and behaviors regarding pain, physical movement and healthcare utilization [11]. PNE studies aimed at non-patients (school children and general population), have shown increased knowledge of pain as well as healthier beliefs and attitudes regarding pain, including more interest in pursuing non-pharmacological treatments [3, 12]. From a psychological perspective, PNE research has demonstrated positive impacts on pain catastrophization and fear-avoidance, shifting individuals to a positive outlook, optimism and goals, which in turn has been associated with a positive recovery and future outlook [11, 13]. It is thus hypothesized that pre-emptive PNE, i.e. PNE delivered to individuals prior to or outside of a painful experience, may set the stage for understanding, realistic expectations, and self-efficacy, which in turn reduces the potential for chronic pain and disability, as well as healthcare utilization including drug-seeking behaviors [14, 15].
In line with this research, scientists recently developed, validated and tested a PNE curriculum for middle school children [3]. In this study, a healthcare provider (physical therapist) delivered a PNE presentation (slides and lecture) to classrooms of middle school children, and measured their knowledge of pain and attitudes and beliefs regarding pain before and after. The results showed that 5th through 8th grade middle school children are able to understand the neurobiology and neurophysiology of pain (increased knowledge), and also shift their attitudes and beliefs regarding pain [3]. However, in order to truly test and impact the PNE program for middle school children, live, healthcare provider-led education is limited in terms of practicality, cost and scalability. This is well documented as potential barriers to mass education [16].
In line with the previous middle school study and the need to test the potential scalability of PNE in schools, this study set out to test if a video-delivery of PNE would result in similar positive findings as the original PNE lecture delivered in-person by a healthcare provider. If the video-delivered PNE lecture were to yield similar results, it may in fact provide an opportunity to deliver a consistent message that is scalable.
Methods
I Particiants and Recruitment
In order to replicate the previous study, a convenience sample of private and public middle schools (5th to 8th grade) in Wisconsin were contacted to participate in the study [3]. Internal Review Board approval was obtained from the University of South Dakota. School administrators were provided with the goals of the study, layout and necessary examples of the proposed lecture and outcome measures. Six schools approved the study and upon approval, teachers were instructed and familiarized with the intended study and the one-time 45-minute session (30 minutes PNE [live or video] and 15 minutes data collection) slotted into their class schedules. Parents were informed about the study and were asked to sign a consent form on the behalf of their children. Participation was entirely voluntary. The PNE lecture/video was set to be delivered in the assigned classroom for each class, resulting in class sizes < 30. The only exclusions set for the study were students who did not want to attend the class, parents objecting to their child attending the class, or not proficient in writing and reading English (per teacher assessment). Classes were randomly assigned by envelope system to either receive a live PNE or video-delivered PNE (Figure1).
Figure 1: Flowchart of the study
II Intervention
The content of PNE is well documented and in line with other studies [3, 17-20]. For the in-person, live presentation and given the short duration of the class period, an abbreviated 30-minute, 32-slide PowerPoint presentation was developed, allowing ample time for survey completion prior to and following the PNE lecture. The PowerPoint presentation's main themes included a discussion of peripheral sensitization, central sensitization, bio-psycho-social factors associated with pain, threat appraisal of the brain, nociception, stress and endocrine responses in pain as well as various therapeutic endogenous strategies to ease pain [17-20]. Various images, metaphors and examples were used to convey the PNE to the students [21]. Following the formal presentation by one of the authors and completion of the post-PNE surveys, participants were encouraged to ask questions. The presentation did not specifically address or target any questions contained in the outcome measures. The PNE-video utilized the exact same content as the live PowerPoint presentation and was a voice-over of the live content along with animated versions of the various images used in the live-presentation. The duration of the video was 30 minutes.
III Outcome Measures
Prior to formal outcome measures, students completed a demographic section capturing their age, gender, grade and participation in sports. Additionally, the demographic survey also enquired about various personal aspects pertaining to pain including currently experiencing pain; past experiences with pain; and family with persistent pain. No personally identifiable information was captured, and pages were coded to allow matching pre- and post-education surveys. Two outcome measures were used for the students to examine their knowledge of pain, and attitudes and beliefs about persistent pain:
Pain Knowledge: Pain knowledge was measured using the revised neurophysiology of pain questionnaire (NPQ). The NPQ is based on a current pain science text and was used in a previous middle school study measuring the neurophysiology knowledge of children [22, 3]. The original NPQ is a 19-item questionnaire requesting 'true#39;; #39;false#39;; or #39; not sure#39; answers to statements, with higher scores indicating more correct answers. Since the development of the NPQ a statistical analysis of the NPQ has led to the development of an abbreviated NPQ with 13 questions which removed ambiguous questions [23]. The revised 13-question rNPQ was used in this study. The questionnaire was adapted similar to a previous study to make it easier for students to understand, e.g., #34;nociception#39; was replaced with #34;danger messages#39; [17]. The authors acknowledge that the 13-point rNPQ has since replaced by a 12-point rNPQ, but the data for this study was collected prior to the 12-point NPQ [24]. No information is available on what constitutes a meaningful shift in NPQ or rNPQ score. The previous middle school PNE study resulted in rNPQ scores improving from 29.5% to 60.8% (31.3% increase) [3].
Pain Beliefs: Healthcare provider#39;s attitudes and beliefs regarding chronic low back pain are often measured with the Health Care Provider#39; s Pain and Impairment Relationship Scale (HC-PAIRS) [25]. This scale has not been used for non-medically trained people or middle school children. Upon review of the HC-PAIRS and the aims of the study, a series of numeric rating scale questions pertaining to beliefs about pain were established by the authors for this study. The numeric rating scale was anchored between 0 (strongly disagree) and 10 (strongly agree). Five questions were established to allow surveys to be completed prior to and following the PNE session in the allotted time. Beliefs statements were:
- Pain is normal; without being able to feel pain you will not survive
- Pain means something is wrong with your tissues
- Pain always means you have to stop what you are doing
- You can control how much pain you feel
- Your brain decides if you feel pain, not your tissues
Both the NPQ and the beliefs numeric scale were administered before and after the PNE lecture/video. To avoid influencing answers to the outcome measures, any questions that arose during the completion of these forms were addressed by the attending teachers and not the presenter of the PNE. Upon completion of the surveys, the surveys were placed into envelopes, sealed and sent to an independent research assistant who entered the data into an Excel document for analysis.
IV Statistical analysis
Analysis of the data was performed with SPSS (version 22.0, IBM Corporation). Descriptive statistics of means, standard deviations, and percentages were reported on the student participant population characteristics. Mann-Whitney U test was performed for between group differences for the outcome measures of pain beliefs questions and pain knowledge after the intervention. Within group measurement changes from pre to post education were tested with Wilcoxon matched pairs signed rank test. Effect size was calculated by r = z /?N, and interpreted at .2 representing a small change, .5 moderate change, and .8 representing a large change [26]. Level of significance was set at p < 0.05.
Results
I Students
A total of 251 middle school students, 5th through 8th grade, completed either a live or video recorded PNE training session. All students completed both pre and posttest questionnaires with some missing data points within various questions, which is shown by the individual n-values reported for each outcome measurement calculation. Complete-case analysis was used for statistical modeling of each individual analysis as two or less data points were incomplete for any individual analysis. Descriptive statistics of the student participants is provided in (Table 1). There was a statistical difference, t(246)=7.21, p<.001, for the mean age of the video group compared with the live group. There was no difference between gender and currently experiencing pain between groups.
Table 1: Participant Characteristics
|
Characteristics |
Live (n=147) |
Video (n=104) |
|
Mean age (years) (SD) |
12.8 (1.1) |
11.8 (1.1) |
|
Female (%) |
79 (53.7) |
55 (52.9) |
|
Grade |
|
|
|
5th |
13 (8.8) |
16 (15.4) |
|
6th |
31 (21.1) |
32 (30.8) |
|
7th |
33 (22.4) |
36 (34.6) |
|
8th |
69 (46.9) |
20 (19.2) |
|
Currently experiencing pain |
40 (27.2) |
41 (39.4) |
|
Previous pain experiences lasting |
|
|
|
None |
2 (1.4) |
1 (1.0) |
|
A week |
67 (45.6) |
47 (45.2) |
|
A month |
41 (27.9) |
32 (30.8) |
|
More than 3 months |
30 (20.4) |
18 (17.3) |
Figure 2: rNPQ scores before and after the live and video presentations
II Pain knowledge and beliefs
Significant changes were found in both groups when comparing within group differences for pre and posttest performance on pain knowledge and pain beliefs questions. (Table 2) The largest effect size was found with changes in pain knowledge in both the live and video PNE sessions. The live session showed an average increase of 4 points on the rNPQ (increase of 31% from 29.8% to 60.8%), while the video session showed an average score increase of 3 points (increase of 23.6% from 25.2% to 48.8%) (Figure 2). Pain beliefs questions of #34;You can control how much pain you feel#34;and #34;Your brain decides if you feel pain, not your tissues#34; both had significant changes in scores with moderate effect size changes in the student beliefs for both groups. Pain belief question, #34;Pain is normal; without being able to feel pain you will not survive#34;, did have a significant change for both group, but the effect size was small. The pain belief question of #34;Pain means something is wrong with your tissues#34; did not see any significant change for either group from pre to post testing. #34;Pain always means you have to stop what you are doing#34; belief question found a significant change in the live group, but it demonstrated a small effect size and no change in the video group.
Table 2: Pre and post education differences for Live and Video groups
|
|
|
Mean (SD) Pre-PNE |
Mean (SD) Post-PNE |
Pre-Post PNE Change |
p-value |
Effect size (r) |
|
Pain Beliefs #1 |
Live (n=146) |
7.07 (2.90) |
7.85 (3.00) |
.78 |
.004 |
.24 |
|
|
Video (n=102) |
6.19 (2.89) |
7.73 (3.23) |
1.54 |
<.001 |
.41 |
|
Pain Beliefs #2 |
Live (n=147) |
4.47 (2.50) |
4.18 (3.46) |
-.29 |
.481 |
-.06 |
|
|
Video (n=103) |
4.30 (2.62) |
4.18 (3.35) |
.12 |
.558 |
-.06 |
|
Pain Beliefs #3 |
Live (n=146) |
2.78 (2.78) |
2.24 (2.77) |
.54 |
.039 |
-.17 |
|
|
Video (n=102) |
2.64 (2.50) |
2.78 (2.66) |
.14 |
.711 |
.04 |
|
Pain Beliefs #4 |
Live (n=146) |
4.24 (3.12) |
6.63 (3.31) |
2.39 |
<.001 |
.51 |
|
|
Video (n=103) |
4.10 (3.21) |
5.98 (3.44) |
1.88 |
<.001 |
.45 |
|
Pain Beliefs #5 |
Live (n=146) |
6.48 (2.95) |
9.42 (1.47) |
2.94 |
<.001 |
.68 |
|
|
Video (n=103) |
6.09 (3.06) |
8.53 (2.50) |
2.44 |
<.001 |
.56 |
|
rNPQ |
Live (n=147) |
3.87 (2.21) |
7.90 (1.99) |
4.03 |
<.001 |
.82 |
|
|
Video (n=104) |
3.27 (1.81) |
6.22 (1.88) |
2.95 |
<.001 |
.81 |
Pain Beliefs #1= Pain is normal; without being able to feel pain you will not survive, Pain Beliefs #2=Pain means something is wrong with your tissues, Pain Beliefs #3=Pain always means you have to stop what you are doing, Pain Beliefs #4=You can control how much pain you feel, Pain Beliefs #5=Your brain decides if you feel pain, not your tissues, rNPQ=Neurophysiology pain questionnaire
Table 3: Live versus Video group differences after education
|
|
|
Mean (SD) |
z-score |
p-value |
Effect size (r) |
|
Pain Beliefs #1 |
Live (n=146) |
7.85 (3.00) |
-.08 |
.936 |
-.01 |
|
Video (n=103) |
7.73 (3.23) |
|
|
|
|
|
Pain Beliefs #2 |
Live (n=147) |
4.18 (3.46) |
.11 |
.912 |
.01 |
|
|
Video (n=103) |
4.18 (3.35) |
|
|
|
|
Pain Beliefs #3 |
Live (n=147) |
2.24 (2.77) |
2.03 |
.042 |
.13 |
|
|
Video (n=103) |
2.78 (2.66) |
|
|
|
|
Pain Beliefs #4 |
Live ((n=147) |
6.63 (3.31) |
-1.46 |
.146 |
-.02 |
|
|
Video (n=103) |
5.98 (3.44) |
|
|
|
|
Pain Beliefs #5 |
Live (n=147) |
9.42 (1.47) |
-3.85 |
<.001 |
-.24 |
|
|
Video (n=103) |
8.53 (2.50) |
|
|
|
|
NPQ |
Live (n=147) |
7.90 (1.99) |
-6.43 |
<.001 |
-.41 |
|
|
Video (n=104) |
6.22 (1.88) |
|
|
|
Pain Beliefs #1= Pain is normal; without being able to feel pain you will not survive, Pain Beliefs #2=Pain means something is wrong with your tissues, Pain Beliefs #3=Pain always means you have to stop what you are doing, Pain Beliefs #4=You can control how much pain you feel, Pain Beliefs #5=Your brain decides if you feel pain, not your tissues, rNPQ=Neurophysiology pain questionnaire
When looking at between group differences of the live and video PNE session (Table 3) there was no difference in the mode of educational delivery for pain beliefs questions 1, 2, and 4. We did find a significant difference favoring the live session for pain beliefs questions 3 and 5, but they were only small effect sizes. Pain knowledge also found the live session producing significantly better scores in pain knowledge, but again only a small effect size.
Discussion
The results from the randomized trial shows that video-delivery of PNE result in comparable changes in pain knowledge and various pain beliefs to live in-person delivered PNE in middle school children.
According to the World Health Organization (WHO) there is a global epidemic of pain, especially chronic pain [27, 28]. Whenever nations and the global community face epidemics, mass, large scale education is often employed[16]. In order to execute a mass education strategy, information shared with populations must be consistent, easy to disseminate and cost-effective[16]. The results from this study provide a step in that direction, showcasing the delivery of PNE via a video being similarly effective as live, in-person delivery of the message. Both groups showed a significant improvement in pain knowledge, not statistically different, and both yielding large effect sizes. The increase in rNPQ was similar to the previously published school NPQ study, while the 23.6% increase in the video group was comparable to patient and healthcare provider studies after PNE [11, 29]. Similarly, both the video and live group had equal shifts in various pain beliefs which yielded moderate effect sizes. The comparable results between video and live presentations suggests that a consistent message can be delivered in a cost-effective and scalable manner, all of which is needed to truly study the effect of mass PNE education for the current pain and opioid epidemic [3, 14]. A key element of the PNE presentations (live and video) is the notion of self-care and self-efficacy, which is in contrast to the current pharmacological approach to dealing with pain. In both groups, students had a significant positive shift that "they control" how much pain they experience (pain belief 4), and both video and live yielded large effect size. This is encouraging, considering the exposure of children and adolescents to passive, potentially harmful pharmacological-only approaches to pain management [5-7]. In contrast, and in line with the content of the PNE messaging in this study, non-pharmacological approaches of pain management (movement, relaxation, meditation, knowledge, sleep hygiene, etc.), should become a focus of the messaging to the general population, including children, which may drive future choices when faced with a painful experience.
The fact that the live presentation yielded larger shifts in pain knowledge and also in pain beliefs # 3 and 5, is not surprising. In clinical studies utilizing education to elicit behavior changes, it is overwhelmingly accepted and proven that one-on-one education is superior to small and large group education, as well as passive educational strategies such as psychoeducational booklets, videos, etc. [11, 29-31]. Current PNE studies evaluating group versus one-on-one education confirms these results[11]. The dilemma, however, is the ability to touch the large number of people suffering from pain, as well as those not in pain yet, i.e., preemptive PNE for school children and the general population[12]. In a study investigating PNE, Moseley (2003) showed that even though one-on-one live PNE yielded superior results compared to a group PNE session, the group session yielded a significant cost savings (decreased number of physical therapy visits), which will over time become increasingly important as the world grapples with the increased financial demands of chronic pain [32]. The results of this study, even though done on middle school children, may additionally yield pathways to deliver PNE at a much larger scale to the general population as a whole. It is well documented that past pain experiences powerfully influence future pain experiences and in this study approximately one in three students were experiencing pain at the time of the study, while nearly one in four has experienced pain lasting more than 3 months. This would imply that how these children learn to think about and develop beliefs about pain (including what to do about it), may powerfully influence future pain experienced and related care choices [33-36]. Early education is key and the results from this study showcase the ability to positively influence pain knowledge as well as various beliefs regarding pain.
This study contains various limitations and opportunities. The video-delivery of PNE is only one audiovisual medium and other mediums of educational delivery may be tested to determine the optimal experience for middle school children. This study does not answer questions in regards to optimal dosage -duration, frequency, etc. of the educational exposure and should be explored in future studies. Outcome measures were only done immediately post-education, not long-term. Only two measures (pain knowledge and beliefs regarding pain) was assessed.
Conclusion
The results from this study shows that a video presentation of PNE yield similar results to live PNE presentations in regards to positively influence pain knowledge and beliefs regarding pain in middle school children. These video results may allow for a consistent, cost-effective and scalable message to middle school kids about pain.
Funding and Grants
This work was supported by a grant from the Iowa Physical Therapy Association (IPTA).
Article Info
Article Type
Research ArticlePublication history
Received: Thu 06, Jun 2019Accepted: Wed 03, Jul 2019
Published: Fri 19, Jul 2019
Copyright
© 2023 Adriaan Louw. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.PDR.2019.02.03
Author Info
Patricia Benz Adriaan Louw Anne Kruse Colleen Louw Jessie Podolak Kory Zimney
Corresponding Author
Adriaan LouwInternational Spine and Pain Institute, PO Box 232, Story City, IA 50248
Figures & Tables
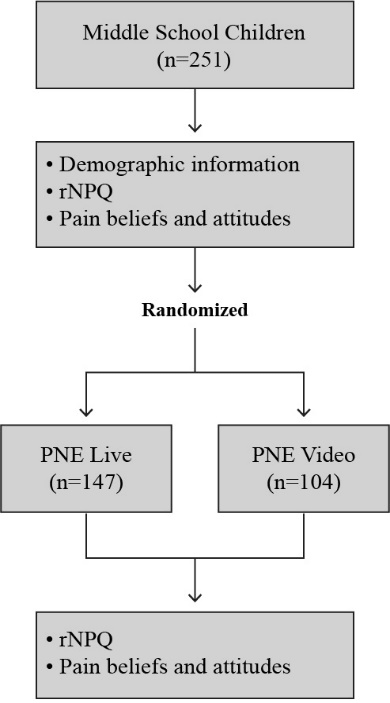

Table 1: Participant Characteristics
|
Characteristics |
Live (n=147) |
Video (n=104) |
|
Mean age (years) (SD) |
12.8 (1.1) |
11.8 (1.1) |
|
Female (%) |
79 (53.7) |
55 (52.9) |
|
Grade |
|
|
|
5th |
13 (8.8) |
16 (15.4) |
|
6th |
31 (21.1) |
32 (30.8) |
|
7th |
33 (22.4) |
36 (34.6) |
|
8th |
69 (46.9) |
20 (19.2) |
|
Currently experiencing pain |
40 (27.2) |
41 (39.4) |
|
Previous pain experiences lasting |
|
|
|
None |
2 (1.4) |
1 (1.0) |
|
A week |
67 (45.6) |
47 (45.2) |
|
A month |
41 (27.9) |
32 (30.8) |
|
More than 3 months |
30 (20.4) |
18 (17.3) |
Table 2: Pre and post education differences for Live and Video groups
|
|
|
Mean (SD) Pre-PNE |
Mean (SD) Post-PNE |
Pre-Post PNE Change |
p-value |
Effect size (r) |
|
Pain Beliefs #1 |
Live (n=146) |
7.07 (2.90) |
7.85 (3.00) |
.78 |
.004 |
.24 |
|
|
Video (n=102) |
6.19 (2.89) |
7.73 (3.23) |
1.54 |
<.001 |
.41 |
|
Pain Beliefs #2 |
Live (n=147) |
4.47 (2.50) |
4.18 (3.46) |
-.29 |
.481 |
-.06 |
|
|
Video (n=103) |
4.30 (2.62) |
4.18 (3.35) |
.12 |
.558 |
-.06 |
|
Pain Beliefs #3 |
Live (n=146) |
2.78 (2.78) |
2.24 (2.77) |
.54 |
.039 |
-.17 |
|
|
Video (n=102) |
2.64 (2.50) |
2.78 (2.66) |
.14 |
.711 |
.04 |
|
Pain Beliefs #4 |
Live (n=146) |
4.24 (3.12) |
6.63 (3.31) |
2.39 |
<.001 |
.51 |
|
|
Video (n=103) |
4.10 (3.21) |
5.98 (3.44) |
1.88 |
<.001 |
.45 |
|
Pain Beliefs #5 |
Live (n=146) |
6.48 (2.95) |
9.42 (1.47) |
2.94 |
<.001 |
.68 |
|
|
Video (n=103) |
6.09 (3.06) |
8.53 (2.50) |
2.44 |
<.001 |
.56 |
|
rNPQ |
Live (n=147) |
3.87 (2.21) |
7.90 (1.99) |
4.03 |
<.001 |
.82 |
|
|
Video (n=104) |
3.27 (1.81) |
6.22 (1.88) |
2.95 |
<.001 |
.81 |
Pain Beliefs #1= Pain is normal; without being able to feel pain you will not survive, Pain Beliefs #2=Pain means something is wrong with your tissues, Pain Beliefs #3=Pain always means you have to stop what you are doing, Pain Beliefs #4=You can control how much pain you feel, Pain Beliefs #5=Your brain decides if you feel pain, not your tissues, rNPQ=Neurophysiology pain questionnaire
Table 3: Live versus Video group differences after education
|
|
|
Mean (SD) |
z-score |
p-value |
Effect size (r) |
|
Pain Beliefs #1 |
Live (n=146) |
7.85 (3.00) |
-.08 |
.936 |
-.01 |
|
Video (n=103) |
7.73 (3.23) |
|
|
|
|
|
Pain Beliefs #2 |
Live (n=147) |
4.18 (3.46) |
.11 |
.912 |
.01 |
|
|
Video (n=103) |
4.18 (3.35) |
|
|
|
|
Pain Beliefs #3 |
Live (n=147) |
2.24 (2.77) |
2.03 |
.042 |
.13 |
|
|
Video (n=103) |
2.78 (2.66) |
|
|
|
|
Pain Beliefs #4 |
Live ((n=147) |
6.63 (3.31) |
-1.46 |
.146 |
-.02 |
|
|
Video (n=103) |
5.98 (3.44) |
|
|
|
|
Pain Beliefs #5 |
Live (n=147) |
9.42 (1.47) |
-3.85 |
<.001 |
-.24 |
|
|
Video (n=103) |
8.53 (2.50) |
|
|
|
|
NPQ |
Live (n=147) |
7.90 (1.99) |
-6.43 |
<.001 |
-.41 |
|
|
Video (n=104) |
6.22 (1.88) |
|
|
|
Pain Beliefs #1= Pain is normal; without being able to feel pain you will not survive, Pain Beliefs #2=Pain means something is wrong with your tissues, Pain Beliefs #3=Pain always means you have to stop what you are doing, Pain Beliefs #4=You can control how much pain you feel, Pain Beliefs #5=Your brain decides if you feel pain, not your tissues, rNPQ=Neurophysiology pain questionnaire
References
- Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, Bohnen AM, van Suijlekom-Smit LW et al. (2000) Pain in children and adolescents: a common experience. Pain 87: 51-58. [Crossref]
- van Dijk A, McGrath P, Pickett W, VanDenKerkhof EG (2006) Pain prevalence in nine- to 13-year-old schoolchildren. Pain Res Manag 11: 234-240. [Crossref]
- Louw A, Podalak J, Zimney K, Schmidt S, Puentedura EJ (2018) Can pain beliefs change in middle school students? A study of the effectiveness of pain neuroscience education. Physiother Theory Pract 34: 542-550. [Crossref]
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP et al. (2015) Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain 156: 569-576. [Crossref]
- Groenewald C and Palermo T (2016) Legitimate opioid prescription increases the risk for future opioid misuse in some adolescents. Evid Based Nurs 19: 83. [Crossref]
- Monitto CL, Hsu A, Gao S, Vozzo PT, Park PS et al. (2017) Opioid Prescribing for the Treatment of Acute Pain in Children on Hospital Discharge. Anesth Analg 125: 2113-2122. [Crossref]
- Yang YT, Chen B, Bennett CL (2016) FDA Approval of Extended-Release Oxycodone for Children with Severe Pain. Pediatrics 137. [Crossref]
- Tian F, Guittar P, Moore-Clingenpeel M, Higgins G, Ardoin SP et al. (2018) Healthcare Use Patterns and Economic Burden of Chronic Musculoskeletal Pain in Children before Diagnosis. J Pediatr 197: 172-176. [Crossref]
- Collins J, Haynes N, Klingberg H, Nicholas H, Pounder M et al. (2017) The Management of Complex Pain in Children Referred to a Pain Clinic at a Tertiary Children's Hospital in Australia. J Orthop Sports Phys Ther 47: 806-813. [Crossref]
- Institute of Medicine (US) Committee on Advancing Pain Research Care and Education (2011) Relieving pain in America: A blueprint for transforming prevention, care, education, and research. National Academies Press. [Crossref]
- Louw A, Zimney K, Puentedura EJ, Diener I (2016) The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract 2016: 332-355. [Crossref]
- Louw A, Zimney K, Puentedura E (2016) Retention of pain neuroscience knowledge: a multi-centre trial. New Zealand J Physiother 44: 91-96.
- Vlaeyen JW, Crombez G, Linton SJ (2016) The fear-avoidance model of pain. Pain 157: 1588-1589. [Crossref]
- Louw A, Puentedura EJ, Zimney K, Schmidt S (2016) Know Pain, Know Gain? A Perspective on Pain Neuroscience Education in Physical Therapy. J Orthop Sports phys ther 46: 131-134. [Crossref]
- Louw A, Diener I, Landers MR, Puentedura EJ (2014) Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine 39: 1449-1457. [Crossref]
- Buchbinder R and Jolley D (2004) Population based intervention to change back pain beliefs: three year follow up population survey. BMJ 328: 321. [Crossref]
- Moseley GL (2003) Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain 4: 184-189. [Crossref]
- Louw A, Butler DS, Diener I, Puentedura EJ (2013) Development of a preoperative neuroscience educational program for patients with lumbar radiculopathy. Am J Phys Med Rehabilb 92: 446-452. [Crossref]
- Louw A (2014) Therapeutic neuroscience education via e-mail: a case report. Physiother Theory pract 30: 588-596. [Crossref]
- Zimney K, Louw A, and Puentedura EJ, Use of Therapeutic Neuroscience Education to address psychosocial factors associated with acute low back pain: a case report. Physiother Theory Pract 30: 202-209. [Crossref]
- Louw A (2013) Why Do I Hurt? A Neuroscience Approach to Pain. Minneapolis: OPTP.
- Wall PD and R Melzack (2005) Textbook of Pain. 5th edn ed. London: Elsevier.
- Catley MJ, O'Connell NE, Moseley GL (2013) How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain 14: 818-827. [Crossref]
- Catley MJ, O'Connell NE, Moseley GL (2013) How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain 14: 818-827. [Crossref]
- Latimer J, Maher C, Refshauge K (2004) The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain 20: 45-50. [Crossref]
- Cohen J (1988) Statistical power analysis for the behavioral sciences. Hilsdale. NJ: Lawrence Earlbaum Associates 2.
- Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386: 743-800. [Crossref]
- Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ, 81: 646-656. [Crossref]
- Moseley GL (2003) Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain 4: 184-189. [Crossref]
- McGregor AH, Doré CJ, Morris TP, Morris S, Jamrozik K (2011) ISSLS prize winner: Function After Spinal Treatment, Exercise, and Rehabilitation (FASTER): a factorial randomized trial to determine whether the functional outcome of spinal surgery can be improved. Spine 36: 1711-1720. [Crossref]
- Louw A, Diener I, Butler DS, Puentedura EJ (2013) Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiother Theory Pract 29: 175-194. [Crossref]
- Moseley GL (2003) Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap 11: 88-94.
- Taddio A, Katz J, Ilersich AL, Koren G (1997) Effects of neonatal circumcision on pain response during subsequent routine vaccination. Lancet 349: 599-603. [Crossref]
- ]Boyle GJ, Goldman R, Svoboda JS, Fernandez E (2002) Male circumcision: pain, trauma and psychosexual sequelae. J Health psychol 7: 329-343. [Crossref]
- ]Knaepen L, Patijn J, van Kleef M, Mulder M, Tibboel D et al. (2013) Neonatal repetitive needle pricking: plasticity of the spinal nociceptive circuit and extended postoperative pain in later life. Dev neurobiol 73: 85-97. [Crossref]
- Page MG, Campbell F, Isaac L, Stinson J, Katz J (2013) Parental risk factors for the development of pediatric acute and chronic postsurgical pain: a longitudinal study. J Pain Res 6: 727-741. [Crossref]
