A Novel Negative Pressure Therapy Technique to Manage a Colo-Cutaneous Fistula following Emergency Aortic Surgery
A B S T R A C T
Negative pressure wound therapy (NPWT) is a well-established technique for managing the open abdominal wound. The decision to intentionally leave an abdominal incision open may be required in the aftermath of surgery for intra-abdominal sepsis or where there is concern regarding abdominal compartment syndrome (ACS). Untreated ACS following elective, or emergency abdominal aortic aneurysm repair (AAA) is associated with mortality rates of up to 60% [1]. Management of the open abdomen, particularly in obese patient, is challenging and labour-intensive. The aim of wound management in this setting is to contain drainage, manage the peri-wound skin and facilitate closure of the wound. This case report discusses the successful management of a complex abdominal wound in a morbidly obese patient complicated by a colo-cutaneous fistula following emergency abdominal aortic aneurysm repair.
Case Report
A 52-year-old man with a high body mass index (BMI) (weight 150Kg) was transferred as an emergency from a peripheral hospital with severe back pain and hypotension. A CT scan confirmed a ruptured 8cm abdominal aortic aneurysm (AAA) with a large retroperitoneal haematoma which on review, was deemed unsuitable for endovascular repair.
The patient underwent emergency open AAA repair, consisting of a midline laparotomy and tube graft repair. Due to failure to perfuse the left leg, the patient required further revascularisation via a longitudinal left groin wound using a jump graft from the aortic tube graft to the left common femoral artery (CFA).
Due to a combination of the patient’s obesity and the large retroperitoneal haematoma, it was not possible to close the abdomen at the end of the procedure. An abdominal closure device (Renasys AB Abdominal Dressing Kit, Smith and Nephew, Ireland Ltd) was placed in the open abdominal wound and the patient was returned to the intensive care unit (ICU).
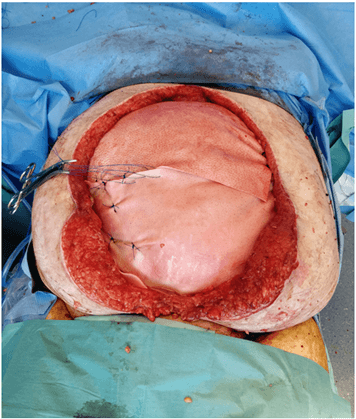
Over the following number of weeks, the patient returned to the theatre for multiple changes of the NPWT dressing and repeated attempts were made to close the abdominal wound. Ultimately the patient underwent placement of a reconstructive tissue matrix to close the wound (Figure 1) (StratticeTM, Allergan PLC, Coolock, Dublin, Ireland). The left groin wound dehisced leaving a large open wound and was managed with NPWT.
The patient had a prolonged ICU admission complicated by myocardial infarction and recurrent episodes of sepsis, including hospital-acquired pneumonia, Staphylococcus aureus PICC line infection and Clostridium difficile infection.
Figure 1: Placement of a reconstructive tissue matrix in the open abdominal wound.
The tissue matrix wound repair was partially successful, but the lower part of the repair failed, and the patient developed a colo-cutaneous fistula involving the sigmoid colon. This made management of the lower part of the abdominal wound particularly difficult. In order to heal both the abdominal wound and the adjacent left groin wound, it was necessary to devise a wound management system that diverted liquid faeces away from the wound while continuing to facilitate wound closure using NPWT.
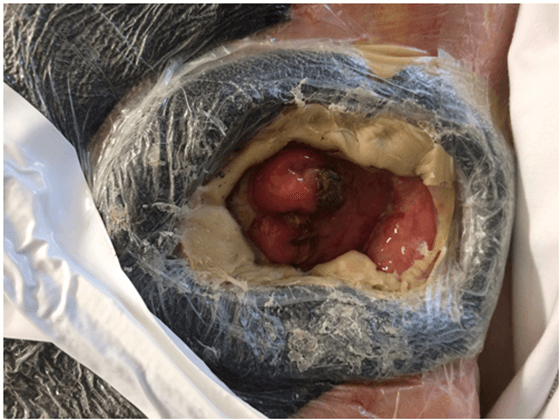
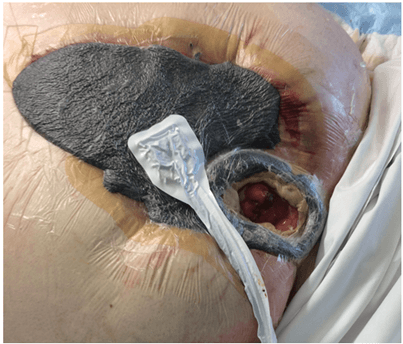
The abdominal wound and fistula were managed by first isolating the faecal fistula using a doughnut shaped piece of gauze (Figure 2) fixed in place around the opening of the colonic fistula with stoma paste. A standard osteomy bag was fixed in place to this doughnut. This facilitated drainage of the faecal stream away from the wound and protected the surrounding skin while allowing concurrent healing of the abdominal and groin wounds using NPWT (Renasys, Smith and Nephew, Ireland Ltd.) (Figure 3).
Figure 2: Isolation of the colo-cutaneous fistula from the abdominal and groin wound using a doughnut-shaped piece of open cell foam. Stoma paste was used to keep this in place and a standard stoma bag was put in place.
Figure 3: Negative pressure was applied to the open abdominal wound while the colo-cutaneous fistula remained isolated.
This wound management system made nursing care of the patient much less labour-intensive and allowed for his discharge to a surgical ward where the dressing was changed every 3 days or sooner if faecal leakage occurred. The patient’s general medical condition improved, and a decision was made not to attempt repair of the colo-cutaneous fistula due to his considerable medical co-morbidities. Instead, the fistula was allowed to mature into a pseudostoma and functioned well. A split skin graft (SSG) was carried out under local anaesthetic using the right leg as a donor site. This was applied to the para-stomal region and kept in place using NPWT.
Over the following number of weeks, the patient had several episodes of small and large bowel obstruction, all managed conservatively with naso-gastric decompression and total parenteral nutrition as repeat laparotomy and definitive repair of the abdominal wall with component separation was deemed too high risk.
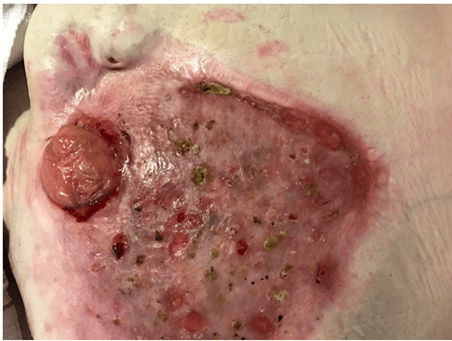
The abdominal wound SSG healed well with some loss of the graft in the para-stomal area. The now isolated sigmoid fistula acted as a formal loop colostomy (Figure 4). The patient made a full recovery and was discharged to a step-down facility on a normal diet.
Figure 4: The colo-cutaneous fistula matured to form a pseudostoma with a healed skin graft on the abdominal wound.
Discussion
Management of the open abdomen is a challenging but life-saving procedure with mortality rates of up to 50% where infection supersedes [2]. The development of an entero-cutaneous fistula into an open abdominal wound poses further risks to their successful management and can profoundly delay and impair healing not only because of direct contamination of the wound but also as a result of malnutrition, electrolyte imbalances and sepsis. Mortality rates of 4.8-20% have been reported in patients with entero-cutaneous fistulae [3]. The objectives of management in these complex cases are to contain fistula drainage, provide a healthy healing environment, avoid peri-stoma skin breakdown and avoid wound contamination [4].
NPWT dressings have been used extensively in the management of these complex wounds due to proven enhancement in wound granulation and wound contracture [5]. However, combining NPWT to the wound with successful drainage of an entero-cutaneous fistula requires individualised and innovative management. Diversion of the gastrointestinal secretions is essential as a first step to avoid wound contamination [3]. Various devices have been used including modified rectal management systems to divert the enteric contents away from the wound and allow wound healing to progress [2, 3, 6].
We describe the use of the NPWT combined with isolation of the fistula in a patient unfit to undergo definitive surgery to correct his fistula and achieve fascial wound closure. Placement of NPWT sponge over the fistula itself without the use of an ostomy appliance will result in the pooling of enteric contents below the sponge resulting in leakage and need for frequent dressing changes. Isolation of the fistula using our technique completely isolates enteric contents from the peri-stomal skin and allows the maturation of granulation tissue to proceed using NPWT.
Wu et al. described a similar technique to that used in our patient using a silicone device to isolate the fistula within the open abdominal wound allowing for separation of the faecal stream from the NPWT dressing [7]. Reed et al. describe a technique almost identical to ours using a crescent-shaped piece of open cell foam dressing placed around the fistula orifice onto which a colostomy bag was fixed [4]. This allows the output from the fistula to be isolated into the colostomy and protects the wound bed from faecal contamination. It also greatly reduces the frequency of dressings, thereby allowing these patients the ability to sleep and ambulate without frequent disturbance.
In the case described, the patient’s high BMI combined with significant cardiac co-morbidity precluded any attempt at definitive surgery to excise the colonic fistula and achieve fascial closure of the wound. The aim, therefore, was to obtain skin closure to prevent sepsis and evisceration.
Conclusion
Different techniques can be utilised for the management of non-surgical fistulae, but the primary goals remain the same. These include isolation and diversion of faecal material and protection of the peri-wound skin and promotion of new granulation tissue to facilitate wound closure.
Careful assessment of the wound and fistula is a key factor in determining the appropriate technique to be used for wound care and wound management. This case describes an innovative adaptation of negative pressure wound therapy with an individualised approach to managing an abdominal wound complicated by a concomitant fistula.
Consent
Written informed consent was obtained from the patient whose case is discussed in the paper regarding publication of this case and accompanying photographs.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Sat 05, Nov 2022Accepted: Mon 21, Nov 2022
Published: Tue 13, Dec 2022
Copyright
© 2023 Mary C. Barry. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2022.04.02
Author Info
Corresponding Author
Mary C. BarryDepartment of Vascular Surgery, St. Vincent’s University Hospital, Elm Park, Ireland
Figures & Tables
References
1.
Rubenstein C, Bietz
G, Davenport DL, Winkler M, Endean ED (2015) Abdominal compartment syndrome
associated with endovascular and open repair of ruptured abdominal aortic
aneurysms. J Vasc Surg 61: 648-654. [Crossref]
2.
Yetisir F, Sarer
AE, Acar HZ (2015) Management of Necrotizing Fasciitis and Fecal Peritonitis
following Ostomy Necrosis and Detachment by using NPT and Flexi-Seal. Case
Rep Surg 2015: 23140. [Crossref]
3.
Hardwicke J, Wright
TC, Hargest R, Dickson W (2010) The use of the Flexi-Seal Faecal Management
System in laparostomy wounds involving enterocutaneous fistula. Ann R Coll
Surg Engl 92: W12-14. [Crossref]
4.
Reed T, Economon D,
Bryant LW (2006) Colocutaneous fistula management in a dehisced wound: a case
study. Ostomy Wound Manage 52: 60-64. [Crossref]
5.
Goverman J, Yelon JA,
Platz JJ, Singson RC, Turcinovic M (2006) The “Fistula VAC,” a technique for
management of enterocutaneous fistulae arising within the open abdomen: report
of 5 cases. J Trauma 60: 428-431. [Crossref]
6. Salgado CJ, Serret MA, Alleyne B, Livingstone AS (2011) Flexi-seal tube use for enteric fistula control in abdominal wall reconstruction. J Plast Reconstr Aesthet Surg 64: 698-702. [Crossref]
7. Wu MH, Wu HY (2009) A simple device for closure of a colo-cutaneous fistula within the laparotomy wound: A Case Report. Ostomy Wound Manage 55: 24-26. [Crossref]
