A Case of Unusual Size Sialolith in the Wharton’s Duct
A B S T R A C T
Sialolithiasis is the common disease of salivary glands. The majority of sialoliths occur in the submandibular gland or the Wharton’s duct. The length of sialolith usually measures from 1 to <10 mm. This article reported a case presenting with sialoliths of a 22mm×15mm in size in the Wharton's duct, which were surgically removed without any complications, and subsequently discusses occurrence factors, signs and symptoms, diagnostic methods and the treatment of sialolithiasis.
Keywords
Sialolithiasis, Wharton’s duct, submandibular gland, transoral sialolithotomy
Introduction
Salivary gland stones are a series of lesions caused by calcified masses in the glands or ducts. About 85% of them occur in the submandibular glands. There is no significant difference in the gender of patients with salivary gland stones. They can occur at any age, but it is more common in young people aged 20-40. The course of the disease can be as short as a few days and as long as several years or even decades [1]. The submandibular gland is one of the major salivary glands, and the obstruction caused by long-term submandibular gland duct stones can cause its secretory function to decrease. Remove the stones in time to eliminate the blockage symptoms, which can promote the recovery of submandibular gland function. Many patients with sialolithiasis involving a duct of a major salivary gland complain of moderate to severe pain, particularly just before, during and after meals, owing to psychic stimulation of salivary flow, associated with swelling of the salivary gland [2]. However, huge stones that occur in the middle of the submandibular duct are relatively rare in clinical practice. In January 2019, the Department of Oral and Maxillofacial Surgery of Hebei Medical University admitted a patient with a duct stone in the left submandibular gland. The stone was approximately 2.2cm×0.8cm×1.5cm, weigh 4.6g, regarded as a huge stone. The report is as follows:
Case Report
I Clinical Data
i. Patient History
The patient was a female, 19 years old, with swelling, pain and discomfort in the left sublingual area for more than 10 years. It was discovered 10 years ago that the left sublingual swelling, pain and discomfort, the swelling and pain increased during eating, symptoms were relieved after oral administration of antibiotics, the swelling frequently increased in the past year, the swelling and pain was obvious one week ago.
ii. Specialist Examination
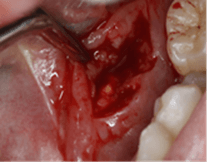
The face is basically symmetrical, and there is no obvious abnormality in the degree of the orifice. Two-handed examination: The left submandibular gland area is palpated with tough texture, unclear borders, and light touch tenderness; the left floor of the mouth is edema, along the direction of the submandibular gland duct, near the sublingual caruncle, palpable mass, hard, clear border, tenderness and tenderness, a small amount of purulent secretion can be seen when squeezing the left gland (Figure 1).
Figure 1: Redness and swelling of the left mandibular fold in the mouth before surgery.
iii. Imaging Examination
Taking a transverse occlusal film of the mandible shows that the middle section of the left submandibular duct can see an oval high-density image (Figure 2).
Figure 2: Sialolith was showed on the transverse occlusal film of the mandible.
iv. Diagnosis
According to the medical history, examination, clinical manifestations and imaging findings, the clinical diagnosis is huge stone in the left submandibular gland, chronic submandibular gland inflammation on the left.
II Treatment Methods
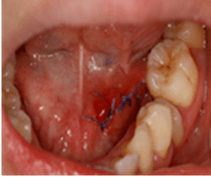
Intraoral local anaesthesia was performed with left submandibular duct incision and lithotripsy; the duct wall was incised along the long axis of the submandibular duct, exposing light yellow stones; inflammatory tissues wrapped around the stones can be seen under the mucosal tissues. At the same time, with a curved vascular clamp, fix the stones. Take out a stone about 2.2cm×0.8cm×1.5cm and weighing 4.6g. Wash away the remaining gravel particles with a large amount of normal saline, intermittently suture the mucosa of the floor of the mouth. Instruct patients to eat more acidic foods to promote saliva secretion and avoid reclogging of the catheter. After the operation, oral anti-inflammatory drugs were taken to prevent infection, and follow-up visits were made on time (Figures 3 & 4).
III Follow-up
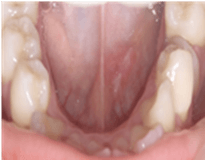
The sutures were removed 1 week after the operation. The wounds healed well. There was no swelling in the left submandibular area when eating, the obstruction disappeared, the left sublingual area was swollen, and the left submandibular area was still palpable with a hard mass; 4 weeks after the operation, re-examination: The swelling in the left sublingual area gradually decreased, and the left submandibular area still had a palpable mass, but the texture gradually became soft, and no secretion was seen from the left catheter port. Re-examination after 12 weeks: The left tongue and the submandibular area are soft, the left submandibular area does not touch the mass, but there is still no secretion out of the left catheter port (Figures 5 & 6).
Figure 3: Sialolith exposed intraoperative incision.
Figure 4: Sialolith was removed during surgery.
Figure 5: 3 days after surgery, local redness and swelling, submandibular region eating swelling subsided.
Figure 6: 3 months after the operation, local mucosa recovered.
Discussion
I The Causes of the Formation of Huge Submandibular Gland Duct Stones
The causes of the formation of huge submandibular gland duct stones were as follows: The mouth of submandibular gland duct is large, and it is easy to enter foreign bodies. Minerals in saliva deposit with foreign bodies as the core and form stones. In addition to the presence of flow against gravity and slower flow rates in the submandibular duct, if the patient does not have symptoms such as severe swelling and pain, or the patient himself has a strong tolerance, thus may lead to prolong the course of the disease and form huge stones [3, 4]. Studies have shown that most of the submandibular gland duct stones are usually 5mm in diameter [5]. Stones can increase at a rate of 1-1.5 mm per year [6]. Stones larger than 15 mm in length or more than 1g in weight are called huge stones [7]. In this case, the stone volume was large, and there were no obvious symptoms in the early stage. The symptoms only appeared in the last week due to local infection. It may be because the course of disease lasted for decades, the calculus was chronic enlarged, the catheter became thicker gradually, and the obstruction symptoms appeared later.
II Correlation Analysis of the Diagnosis and Treatment Process of this Case
The symptoms and signs of patients with submandibular gland duct stones are relatively typical in clinical practice. It is very easy to make a diagnosis by the mandibular transverse occlusal film. According to the literature, 70% of cases can be diagnosed by palpation and examination of the mandibular transverse occlusal film [8-10]. This examination method is simple and low cost, so it can be used as the preferred auxiliary examination method. In recent years, the clinical application of salivary gland lithotomy and extracorporeal lithotripsy has gradually increased, but its cost is high, and it is difficult to popularize in China. In addition, it is difficult to remove stones with large volumes. In the absence of salivary gland endoscopy and lithotripsy equipment, for the stones located in front of the second molars, after double diagnosis, the main method is to take stones through the catheter [11]. Regardless of the course of disease, inflammation and function of the submandibular gland, simple removal of calculus from the mouth is a commonly used method. Some studies have shown that after lithotomy, the submandibular gland duct can be kept unobstructed, which is conducive to the recovery of gland function [12].
Yoshimura et al. reported that 75% of the gland function could be recovered within one year after the operation [13]. In the research of domestic scholars, the recovery rate of gland function within three years is about 75%, but with the extension of postoperative time, the gland function presents a downward trend, and some gland function completely loses. It is a simple and effective method to remove the submandibular gland swelling caused by duct stones. If long-term submandibular gland infection repeatedly causes chronic submandibular gland inflammation, and its secretion function decreases or even disappears, submandibular gland resection is required, and there are many postoperative complications. The patient had a history of more than 10 years and still had submandibular gland enlargement after eating, indicating that the gland still has secretion function. Therefore, the treatment of this case of submandibular gland duct huge stone is to remove the obstruction and promote gland function recovery [14]. At first, we planned to use 99mTc continuous dynamic imaging to observe the functional recovery of the submandibular gland before and after stone removal. However, because the clinical symptoms of the patients have completely disappeared after surgery, and also consider the economic problems, they choose to observe, and further treatment is carried out according to the specific secretion of gland function in the future.
Conclusion
For the huge stones in the middle part of the submandibular gland duct, we can use the method of double diagnosis and the location of mandibular transverse occlusal film to determine the position. It can not only avoid the scar of maxillofacial skin but also promote the recovery of gland function with a high success rate and few complications. After the removal of obstruction factors, the obstruction symptoms disappeared immediately, and the recovery of gland function was significantly improved compared with that before the operation. For patients with submandibular gland inflammation, we can first cut the duct to remove the obstruction, which is conducive to the recovery of gland function.
Acknowledgements
This study was supported by Science and Technology Projects of Hebei Province (no.15277762D) and Health Commission of Hebei Province (no.20180603).
Article Info
Article Type
Case ReportPublication history
Received: Thu 01, Oct 2020Accepted: Mon 19, Oct 2020
Published: Thu 29, Oct 2020
Copyright
© 2023 Zhang Xudong . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.05.04
Author Info
Chen Ruixue Sun Xu Li Xiangjun Zhang Xudong
Corresponding Author
Zhang XudongSchool and Hospital of Stomatology, Hebei Medical University & Hebei Key Laboratory of Stomatology, Shijiazhuang, Hebei Province, China
Figures & Tables



References
- Hammett JT, Walker C (2020) Sialolithiasis. StatPearls. Treasure Island (FL): StatPearls Publishing.
- Parkar MI, Vora MM, Bhanushali DH (2012) A Large Sialolith Perforating the Wharton's Duct: Review of Literature and a Case Report. J Maxillofac Oral Surg 11: 477-482. [Crossref]
- Drage NA, Brown JE, Makdissi J, Townend J (2005) Migrating salivary stones: report of three cases. Br J Oral Maxillofac Surg 43: 180-182. [Crossref]
- Romero NJ, Fuson A, Kieliszak CR, Joshi AS (2019) Sonolocation during submandibular sialolithotomy. Laryngoscope 129: 2716-2720. [Crossref]
- Batori M, Mariotta G, Chatelou H, Casella G, Casella MC (2005) Diagnostic and surgical management of submandibular gland sialolithiasis: report of a stone of unusual size. Eur Rev Med Pharmacol Sci 9: 67-68. [Crossref]
- Iqbal A, Gupta AK, Natu SS, Gupta AK (2012) Unusually large sialolith of Wharton's duct. Ann Maxillofac Surg 2: 70-73. [Crossref]
- Bhullar RS, Dhawan A, Bhullar K, Malhotra S (2015) Giant submandibular gland duct sialolith mimicking an impacted canine tooth. Natl J Maxillofac Surg 6: 89-92. [Crossref]
- Omezli MM, Ayranci F, Sadik E, Polat ME (2016) Case report of giant sialolith (megalith) of the Wharton's duct. Niger J Clin Pract 19: 414-417. [Crossref]
- Sakthivel P, Yogal R, Singh S, Sharma P, Singh CA (2017) Giant Sialolith of Submandibular Duct. JNMA J Nepal Med Assoc 56: 262-264. [Crossref]
- Brown JE (2006) Interventional sialography and minimally invasive techniques in benign salivary gland obstruction. Semin Ultrasound CT MR 27: 465-475. [Crossref]
- Ruiz R, Brygo A, Nicot R, Ferri J (2018) Sialolithiasis removal under general anesthesia: A descriptive retrospective study in the maxillofacial surgery department in Lille University Hospital. J Stomatol Oral Maxillofac Surg 119: 97-101. [Crossref]
- Makdissi J, Escudier MP, Brown JE, Osailan S, Drage N et al. (2004) Glandular function after intraoral removal of salivary calculi from the hilum of the submandibular gland. Br J Oral Maxillofac Surg 42: 538-541. [Crossref]
- Yoshimura Y, Morishita T, Sugihara T (1989) Salivary gland function after sialolithiasis: scintigraphic examination of submandibular glands with 99mTc-pertechnetate. J Oral Maxillofac Surg 47: 704-710. [Crossref]
- Gadve V, Mohite A, Bang K, Shenoi SR (2016) Unusual giant sialolith of Wharton's duct. Indian J Dent 7: 162-164. [Crossref]
