Acceptance and Commitment Therapy for People with Multiple Sclerosis: A NonConcurrent Multiple Baselines Design
A B S T R A C T
Objective: People with multiple sclerosis often suffer from distress, reduced societal participation and low quality of life. Evidence-based psychological treatment options for multiple sclerosis are limited. The aim of this study was to investigate the effectiveness of Acceptance and Commitment Therapy on participation and quality of life for people with multiple sclerosis.
Methods: We performed a non-concurrent multiple baselines design study. Six female patients with multiple sclerosis participated. Randomization was implemented by assigning participants randomly to a baseline (waiting) period of three, six or nine weeks. We measured quality of life, and participation on a daily basis, and acceptance and cognitive defusion on a weekly basis. Statistical analyses were performed using randomization tests.
Results: After Acceptance and Commitment Therapy, five participants showed statistically significant increases in quality of life and three participants showed statistically significant improvements in participation. Acceptance increased in two patients, and cognitive defusion improved in one patient.
Conclusion: Acceptance and Commitment Therapy seems promising for improving the quality of life and participation in people with multiple sclerosis. Mechanisms underlying improvement are not clear yet. Further large-scale controlled studies with more representative samples and a longer follow-up period are justified.
Keywords
Behaviour-change strategies, multiple sclerosis, participation, psychological flexibility, quality of life, third generation behavioural therapies
Introduction
Multiple sclerosis (MS) is the most common neurological disorder in young adults. The clinical picture is diverse, with physical and neuropsychiatric symptoms. The course is fluctuating and unpredictable and often progressive [1]. People with MS often suffer from distress and catastrophizing thoughts about the future. Depression and anxiety levels are high, societal participation is reduced, and quality of life (QoL) is low [2-5].
Evidence-based psychological treatment options for people with MS are limited [6, 7]. However, growing evidence suggests that cognitive behavioral therapy (CBT) may be effective [8-10]. Over the last ten years, evidence for the effectiveness of third-generation behavioral therapies, including Acceptance and Commitment Therapy (ACT), is growing. ACT mixes acceptance- and mindfulness-based strategies with commitment and behavior-change strategies to increase acceptance and cognitive defusion. Cognitive defusion is the ability to separate from one’s thoughts to deal with unhelpful or self-defeating beliefs [11]. Several studies with patients with depression, anxiety, diabetes mellitus, cancer or chronic pain link ACT to decreased fatigue, depression and anxiety, and increased participation and QoL [2, 12-17].
The effects of ACT have been studied in people with MS applying several treatment approaches and investigating several outcomes [18-24]. The studies indicate that ACT is a promising method for improving psychological well-being and functioning in everyday life. However, only two uncontrolled design studies used QoL as an outcome measure, and none of the studies investigated effects on participation. The primary aim of the current study was, therefore, to investigate the effectiveness of ACT in people with MS on QoL and participation, using a controlled study design. Second, we investigated whether ACT would increase acceptance and cognitive defusion.
Method
I Study Design
A non-concurrent multiple baselines design was performed, including a baseline, an intervention and a follow-up phase. Randomization was implemented by assigning participants randomly to a baseline (waiting) period of three, six or nine weeks. During the study period, participants received standard medical care (including regular visits to the neurologist and standard medication). The medical ethics committee Z (Zuyderland-Zuyd) approved the study protocol (NL48536.096.14). All participants gave written informed consent.
II Participants
People with MS were recruited from the Zuyderland Medical Center between April 2014 and June 2015. Patients who started ACT as part of standard clinical practice during the study period were screened for eligibility. Inclusion criteria were: (1) a clinically definite MS diagnosis according to the MacDonald classification criteria; (2) reduced participation as indicated by two or more restrictions on the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P); (3) age between 18 and 65 years; (4) problems accepting the illness (based on clinical judgment) and (5) motivation for an eight-session psychological intervention focusing on acceptance in chronic illness, based on the clinical judgment of a psychologist [25, 26].
Exclusion criteria were: (1) insufficient understanding of the Dutch language; (2) intellectual disability or lack of verbal abstraction, based on educational history and clinical judgment; (3) severe psychiatric disorders (e.g., current severe depressive episode, psychosis, social phobia, delirium, dementia or severe cognitive impairment); (4) MS relapse or corticosteroid use within the past four weeks and (5) former formal treatment based on ACT and/or mindfulness.
III Measures
i Participant Characteristics
Participant characteristics were measured at baseline. Information was collected regarding sex, age, marital status, level of education and employment status. Type of MS, disease duration, comorbidity during the study, and neurological impairment measured with the Expanded Disability Status Scale (EDSS) were extracted from medical files [27]. The EDSS score ranges from zero to ten, where zero indicates a normal neurological examination, and ten indicates death.
To assess cognitive status, three neuropsychological tests were administered. The oral version of the Symbol Digit Modalities Test (SDMT) was used to measure information processing speed. The Paced Auditory Serial Addition Test (PASAT) was used to measure information processing speed, working memory and attention/concentration. The Controlled Oral Word Association Test (COWAT) was used to measure executive functioning. The patient’s cognitive test results were classified as cognitively impaired when z-scores were ≤ -2 on one test, or ≤ -1.5 on two tests. The tests are highly sensitive and reliable for people with MS [28]. The Hospital Anxiety and Depression Scale (HADS) was administered to assess symptoms of depression and anxiety [29]. Both subscales consist of seven items, with scores ranging from 0-21. Higher scores indicate more symptoms. Reliability is demonstrated for the Dutch population, and validity is adequate for people with MS [30, 31].
The subscale subjective fatigue of the Checklist Individual Strength-20 (CIS-20) was administered to assess fatigue [32]. This subscale consists of eight items answered on a seven-point Likert scale. The total score ranges from eight to 56. A score of 35 or higher indicates severe fatigue [33]. Cronbach’s α is .88 in people with MS [34].
ii Primary Outcome Measures on QOL and Participation
QoL was measured daily with a paper Visual Analogue Scale (VAS) and a paper Numerical Rating Score (NRS) [35, 36]. The question “How content are you with your daily life” was answered on a continuous VAS of ten centimeters in length with anchor “absolutely not content” on the left and anchor “completely content” on the right, resulting in a score between 0 and 10. VAS ratings are recommended in clinical trials to assess the global quality of life and have excellent validity and reliability [37]. The NRS was formulated as “Which numeric rating score from 1 (very bad) to 10 (very well) do you give your life in general?”. NRS has high reliability and concurrent validity [38-40].
Participation was measured on a weekly basis with the paper Utrecht Scale for Evaluation of Rehabilitation-Participation [26]. It is divided into three scales assessing frequency of participation (12 items, e.g. “In the last week, how many times did you visit your family or friends”), restrictions to participation (10 items, e.g. “Are you, because of your disease or condition, limited in doing sports or other physical exercise”), and satisfaction with participation (9 items, e.g. “How satisfied are you about the relationship with your partner”). Scale scores are converted to a 0-100 scale with higher scores indicating better participation (i.e. more frequencies, fewer restrictions, higher satisfaction). The USER-P has adequate reliability and validity in patients with physical disabilities [26].
Table 1: Participant characteristics.
|
Participant |
Sex |
Age |
Type MS |
Disease duration in years |
EDSS |
SDMT* |
PASAT* |
COWAT* |
CIS-20 |
HADS -D |
HADS- A |
Comorbity |
|
A |
f |
55 |
RRMS |
3 |
1.5 |
0.5 |
-0.1 |
-0.6 |
44 |
14 |
12 |
Migraine |
|
B |
f |
39 |
RRMS |
3 |
1 |
-0.5 |
-0.5 |
-0.5 |
37 |
13 |
16 |
Diabetes mellitus type I |
|
C |
f |
53 |
RRMS |
6 |
2.5 |
-1.5 |
-1.0 |
-1.7 |
51 |
12 |
15 |
Neuropathic pain |
|
D |
f |
58 |
SPMS |
9 |
6.5 |
-0.3 |
-0.6 |
-1.2 |
47 |
8 |
12 |
Hyperhidrosis and ulcerative colitis |
|
E |
f |
41 |
RRMS |
11 |
4 |
0 |
-0.6 |
-0.9 |
48 |
13 |
16 |
- |
|
F |
f |
50 |
RRMS |
3 |
3.5 |
0.7 |
1.3 |
-0.6 |
49 |
7 |
14 |
- |
*: z-scores
MS: Multiple Sclerosis; SPMS: Secondary Progressive Multiple Sclerosis; RRMS: Relapsing Remitting Multiple Sclerosis; EDSS: Expanded Disability Status Scale; SDMT: Symbol Digit Modalities Test; PASAT: Paced Auditory Serial Addition Test; COWAT: Controlled Oral Word Association Test; CIS-20: subscale fatigue of Checklist Individual Strength-20; HADS-D: subscale depression of the Hospital Anxiety and Depression Scale; HADS-A: subscale anxiety of Hospital Anxiety and Depression Scale.
iii Secondary Outcome Measures Assessing Acceptance and Cognitive Defusion
The Acceptance and Action Questionnaire II (AAQ-II) was administered weekly (on paper) to assess acceptance and experiential avoidance [41]. Answers are scored on a 7-point Likert scale ranging from “never true” (1) to “always true” (7), with higher scores indicating better acceptance. The Dutch AAQ-II has good internal consistency (Cronbach’s α = 0.85) [42]. The Cognitive Fusion Questionnaire (CFQ-13) was administered weekly (on paper) to assess cognitive defusion and consists of 13 items measured on a 7-point Likert scale [43]. Answer options range from “never true” (1) to “always true” (7), with higher scores indicating better cognitive defusion. Internal consistency of the Dutch CFQ-13 is good (Cronbach’s α >0.80) [44].
IV Procedure
People with MS from Zuyderland Medical Center who reported problems with accepting their illness during a regular visit to their neurologist, nurse practitioner or psychologist, visited a consultant in rehabilitation medicine for the referral to ACT treatment as part of standard care. If agreed, the researchers contacted the patients by telephone to provide them with information about the study and to check the inclusion and exclusion criteria. After one to two weeks to think and decide about participation, candidates signed informed consent.
After written consent was given, the baseline measurements took place. All participants started with a waiting period (the baseline phase) in which they received standard medical care. This baseline phase varied in length; participants were randomly assigned to three, six, or nine weeks waiting time. During the baseline phase, participants completed daily and weekly assessments. After the baseline phase, the ACT intervention was carried out for eight weeks. Daily and weekly measures continued during the intervention and lasted until three months after the intervention phase.
V Intervention
The ACT intervention involved eight weekly sessions of two hours [45, 46]. A summary of the content of the ACT protocol is provided in (Appendix Table 1). At the start of the intervention, participants received a workbook with instructions. In addition to the weekly sessions, participants were asked to practice the ACT skills six days a week for about 30 minutes per day. They also could read the Dutch version of the book ‘The Happiness Trap’ (‘De Valstrik van het Geluk’) [47]. For practical reasons, participants started with the intervention consecutively in three groups, which consisted respectively of four, four and two participants.
Each group was led by a certified psychologist/ACT-therapist. She had ten years of experience as a psychologist, three years in ACT therapy, and had worked with people with MS for over five years. She followed an ACT training course of 36 hours, organized by a Dutch accredited institution. She was blinded for the assessment results.
VI Data Analysis
For each participant, QoL data were plotted graphically, and data on QoL, participation, and acceptance and cognitive defusion were analyzed using descriptive statistics (Mean, SD) to allow for visual inspection [48]. In addition, we used randomization tests of the daily assessments of QoL and the weekly assessments of participation and acceptance and cognitive defusion to calculate the statistical significance of the changes in levels across phases (baseline versus intervention plus follow-up).
Theoretically, treatment could be scheduled to start at any of the 210 observation time points in the trial (nine weeks of baseline, eight weeks of intervention and thirteen weeks of follow-up makes 30 weeks of seven days, or 210 days). This was restricted so that both the baseline phase and treatment phase contained at least 21 observations (3 weeks). For practical reasons, randomization over three moments was chosen: for each participant, treatment could start after either three, six, or nine weeks of baseline measurements. Participants assigned to a three-week baseline had 169 observation points (three weeks baseline, eight weeks intervention, thirteen weeks follow-up). Participants assigned to a six-week baseline had 189 observation time points (six weeks baseline, eight weeks intervention, thirteen weeks follow-up). Participants assigned to a nine-week baseline had 210 observation time points (nine weeks baseline, eight weeks intervention, thirteen weeks follow-up).
Randomization tests were used to derive statistics from the observed data. To compare differences between phase scores, t-statistics were used [49]. Furthermore, after the main study tests, the randomization tests were repeated for delayed effects, given that it was a priori unknown how many days would be required after the start of the intervention before significant effects would emerge. Moreover, the rationale behind ACT predicts continuing improvements after therapy has ended. Randomization tests were repeated for each participant to identify the smallest p-value individually [50].
Results
I Participants
During the study period, ten patients started ACT as part of standard clinical practice. All ten patients were eligible and willing to participate in this study. Data of four patients were excluded for analyses for various reasons (too few baseline measures completed; could not start course due to illness; unclear or multiple answers on questionnaires). For the remaining six participants, results were analyzed. See (Table 1) for participant characteristics.
The mean age of participants was 49.3 years (SD 6.9). All participants were females and married or living together with a partner. Three participants experienced no to minimal disabilities due to MS (EDSS < 3), and three participants had moderate to severe disabilities, affecting or impairing their daily activities (EDSS ≥ 3). The level of education was at a medium (n=3) or higher level (n=3). Two participants had a part-time job; the others did not work. All participants reported severe fatigue (CIS-20 subjective fatigue ≥35) and high levels of depression and anxiety (HADS ≥ 8 for the respective subscale). One participant was classified as mildly cognitively impaired. Randomization determined that for participants A and D, treatment started after three weeks of baseline, for participants B and E, after six weeks of baseline, and for participants C and F, after nine weeks of baseline. During the intervention and follow-up phase, participant A missed one assessment day, participant B missed 44 assessment days due to life events, participant D missed nine assessment days due to hospitalization, participant E missed four assessment days, and participants C and F missed no assessments days.
II Primary Outcomes
i Quality of Life
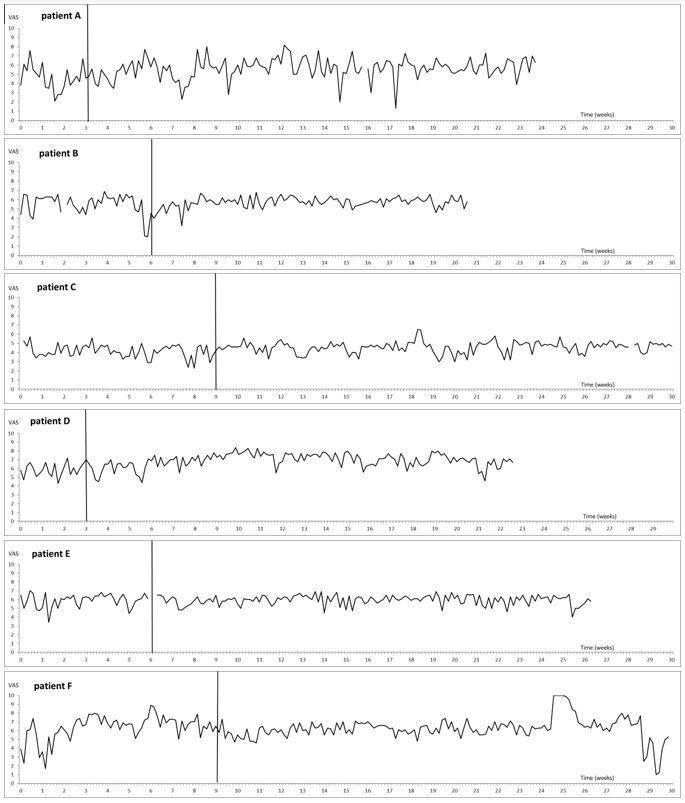
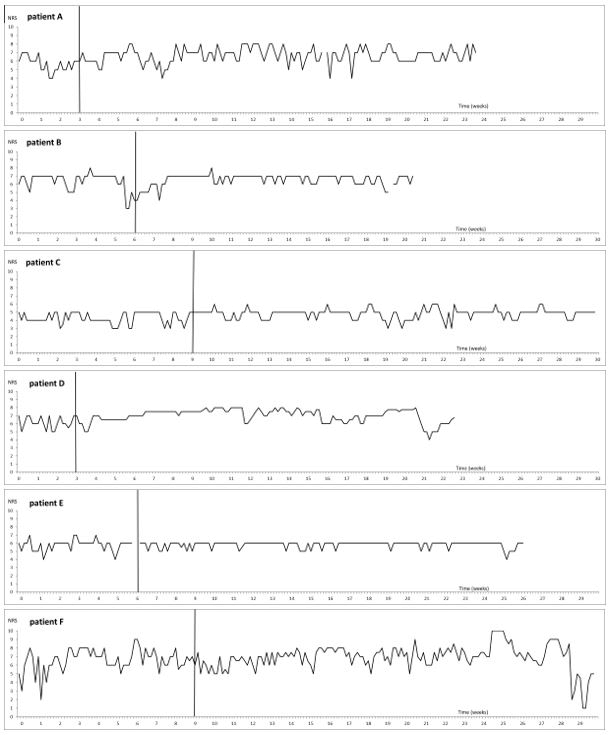
The results on the VAS-QoL are presented in (Figure 1). The results on the NRS-QOL are presented in (Figure 2). Table 2 shows means and SDs per phase.
Figure 1: Daily marks at a Visual Analogue Scale for experienced quality of life per participants A, B, C, D, E and F, over time. The vertical line is the start of the intervention.
Figure 2: Daily marks at a Numerical Rating Score for experienced quality of life per participants A, B, C, D, E and F, over time. The vertical line is the start of the intervention.
Visual inspection of the raw data showed an increase in VAS-QoL for four participants (participants A, B, C and D) and an increase in NRS-QoL for five participants (participants A, B, C, D and F). For three participants QoL scores increased by 10% or more (participants A, C and D). Randomization tests (Table 2) showed a statistically significant immediate increase in VAS-QoL from baseline to intervention plus follow-up phase for participant C (t=0.428, p=0.012). Effects were delayed for participants A (t = 1.120, p = 0.016), B (t = 0.436, p = .0.019) and D (t = 1.182, p = 0.034). NRS-QoL showed a statistically significant immediate increase from baseline to intervention plus follow-up phase for participants A (t = 0.995, p = 0.016) and C (t = 0.568, p = 0.042), and delayed effects for participants B (t = 0.571, p = .0.010), D (t = 1.001, p = 0.009) and F (t = 0.619, p = 0.036).
Table 2: Participants’ baseline and post-treatment scores and randomization test results.
|
Visual Analogue Scale – Quality of Life |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
4.63 (1.35) |
5.63* (1.13) |
0.168 |
0.016** |
10 |
|
B |
5.46 (1.10) |
5.75 (0.54) |
0.417 |
0.019** |
12 |
|
C |
4.14 (0.70) |
4.56* (0.62) |
0.012** |
|
|
|
D |
5.79 (0.75) |
6.89* (0.80) |
0.179 |
0.034** |
22 |
|
E |
5.91 (0.75) |
5.93 (0.55) |
0.762 |
|
|
|
F |
6.37 (1.42 ) |
6.25 (1.26) |
0.917 |
|
|
|
Numerical Rating Score – Quality of Life |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
5.67 (0.89) |
6.66* (0.89) |
0.016** |
|
|
|
B |
6.37 (1.10) |
6.56 (0.71) |
0.476 |
0.010** |
11 |
|
C |
4.25 (0.70) |
4.82* (0.62) |
0.042** |
|
|
|
D |
6.11 (0.74) |
6.99* (0.82) |
0.171 |
0.009** |
9 |
|
E |
5.76 (0.68) |
5.81 (0.40) |
0.566 |
|
|
|
F |
6.59 (1.31) |
6.90 (1.45) |
0.685 |
0.036** |
28 |
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Frequencies |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
12.67 (2.52 ) |
15.57* (2.42) |
0.111 |
|
|
|
B |
14.00 (0.89) |
14.36 (1.55) |
1.000 |
|
|
|
C |
8.56 (1.24) |
7.52 (1.17) |
0.750 |
|
|
|
D |
6.33 (2.89) |
11.40* (4.21) |
0.176 |
|
|
|
E |
11.50 (1.64) |
11.00 (1.45) |
0.200 |
|
|
|
F |
13.11 (1.05) |
11.19 (1.44) |
1.000 |
|
|
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Restrictions |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
51.11 (10.18) |
57.50* (4.57) |
0.063 |
|
|
|
B |
75.00 (5.48) |
79.88 (2.81) |
0.276 |
|
|
|
C |
54.44 (5.27) |
56.51 (5.72) |
0.923 |
0.048** |
42 |
|
D |
46.67 (8.82) |
51.57* (18.58) |
0.126 |
|
|
|
E |
54.44 (1.72) |
54.17 (1.48) |
0.357 |
|
|
|
F |
62.96 (4.84) |
66.98 (1.45) |
0.048** |
|
|
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Satisfaction |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
35.83 (3.82) |
52.50* (7.12) |
0.056 |
|
|
|
B |
45.83 (5.63) |
50.71* (6.89) |
1.133 |
|
|
|
C |
48.19 (3.91) |
47.38 (1.24) |
0.583 |
|
|
|
D |
30.00 (8.66) |
59.94* (17.38) |
0.176 |
|
|
|
E |
42.50 (0.00) |
43.25 (1.18) |
0.900 |
0.050** |
105 |
|
F |
51.11 (1.32) |
58.93* (9.44) |
0.750 |
0.042** |
77 |
|
Acceptance & Action Questionnaire II |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
37.25 (4.66) |
43.35* (2.63) |
0.056 |
|
|
|
B |
40.83 (2.11) |
39.00 (4.12) |
0.867 |
|
|
|
C |
43.22 (1.99) |
41.00 (2.27) |
0.750 |
|
|
|
D |
47.67 (4.78) |
64.00* (2.95) |
0.176 |
|
|
|
E |
54.83 (2.85) |
54.45 (2.62) |
0.950 |
|
|
|
F |
37.89 (4.23) |
47.76* (7.83) |
0.667 |
0.042** |
35 |
|
Cognitive Fusion Questionnaire 13 |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
43.00 (2.92) |
51.05* (3.94) |
0.056 |
|
|
|
B |
50.83 (4.22) |
51.29 (1.98) |
0.733 |
|
|
|
C |
55.44 (3.83) |
54.81 (3.36) |
0.750 |
|
|
|
D |
65.33 (5.73) |
85.55* (4.77) |
0.176 |
|
|
|
E |
67.00 (2.31) |
66.70 (3.07) |
0.850 |
0.050** |
105 |
|
F |
47.11 (2.13) |
62.48* (8.20) |
0.375 |
0.042** |
21 |
*: more than 10% increase from baseline; **: statistically significant increase (p≤0.05); FU: follow-up period; SD: standard deviation.
ii Participation
The mean and standard deviation of the USER-P frequencies, restrictions and satisfaction subscales are shown in (Table 2). For participants A, B and D visual inspection indicates that the mean frequencies score increased over time; for patients A and D, scores increased by more than 10%. Participants C, E and F showed a small decrease in frequency. The mean restrictions score increased (i.e., improved) for participants A, B, C, D and F; for patient A and D scores increased by more than 10%. The mean satisfaction score deteriorated for participant C, while the other participants showed an improvement; for patients A, B, D and F scores increased by more than 10%.
Table 2 displays the results of the randomization tests. Randomization tests showed no significant effects in the USER-P frequency score. The USER-P restrictions score showed a statistically significant immediate increase for participant F from baseline to intervention plus follow-up phase, and a statistically significant delayed effect for participant C. The USER-P satisfaction score showed no statistically significant immediate effects, but showed a delayed increase for participants E and F.
III Secondary Outcomes
Acceptance and Cognitive Defusion
The means and standard deviation of acceptance and experiential avoidance (AAQ-II) and of cognitive defusion (CFQ-13) are shown in (Table 2). Visual inspection showed that for participants A, D and F the mean AAQ-II score increased over time (an increase of more than 10%). Randomization tests showed no immediate improvements, and only participant F had a statistically significant delayed improvement on the AAQ-II (Table 2). Visual inspection further showed that the mean CFQ-13 score increased for participants A, B, D and F; for patients A, D and F scores increased by more than 10%. Randomization tests indicated no immediate statistically significant increases, but delayed increases on the CFQ-13 were statistically significant for participants E and F (Table 2).
Discussion
The main objective of this study was to examine the effectiveness of ACT on QoL and participation in people with MS. Results indicate that ACT may have significant potential to improve QoL and participation in people with MS. Participation improved in three of the six participants. QoL increased in five of the six participants. The results on QoL are in line with the results of other studies on ACT and QoL [18, 24], and on Mindfulness-Based Cognitive Therapy and CBT in people with MS [51, 52]. Improvements in QoL were maintained at follow-up, except when participants were confronted with major life events, which is in line with earlier research [9].
The results for acceptance and cognitive defusion were mixed. Statistical analyses indicated that only two participants experienced significant improvements in acceptance, while cognitive defusion improved significantly in only one patient. However, visual inspection showed that the scores increased by more than 10% for half of the patients. Several possible reasons for these mixed results can be given. First, our follow-up period may have been too short. ACT skills such as acceptance, cognitive defusion and contact with here and now may first have to be incorporated into daily life. Second, in the present study, all participants started with high and clinically significant levels of anxiety, depression and fatigue. The high emotional and physical burden negatively may have influenced treatment adherence leading to less effect on acceptance and defusion.
To the best of our knowledge, this is the first study with a controlled design evaluating the effect of ACT on both QoL and participation in people with MS. The non-concurrent multiple baselines design made it possible to collect data on a daily or weekly basis, enabling high power with only a small number of participants. Although six participants are not a large sample, it exceeds recommendations to use a minimum of four units to maximize the possibility of drawing valid inferences [53, 54].
The study also has some limitations. First, some data could not be used because too few baseline measures were completed, because answers on questionnaires were unclear or because multiple answers were given. Compliance and reliability of the daily measures could be improved by administration via the internet or on a smartphone-app [55]. In the present study, this might have prevented the missing results of two participants. Second, only women remained in the final sample. Although women are overrepresented in the MS population, the disease also affects men. Third, although participants seemed motivated during the sessions, we did not measure treatment adherence or compliance with homework, and no information is available about the time participants spent on reading the workbook and practicing ACT skills. Fourth, previous research showed the benefits of ACT over the long term [9, 42, 52, 56-58]. The three-month period following the end of the intervention is possibly too short to get a realistic view of the lasting effects. Finally, the mechanisms underlying changes in QoL and participation and changes in acceptance and cognitive defusion are not clear yet. Future research into the processes underlying change should further investigate this.
In conclusion, ACT seems to be a promising intervention to improve QoL and participation in people with MS and may be a useful addition to the available pharmacological treatments. Further research should study the mechanisms and effects of ACT in people with MS in controlled designs with longer follow-up periods and with larger patient groups consisting of both men and women.
Highlights
i. Evidence-based psychological treatments for people with MS are scarce.
ii. Acceptance and commitment therapy improve the quality of life of people with MS.
iii. Acceptance and commitment therapy improve the participation of people with MS.
Declarations of Interest
None.
Funding
None.
Appendix Table 1: ACT group protocol: Contents per session.
|
Session |
Core process |
Goal |
During session |
Homework |
|
1 |
Experiental avoidance & Creative hopelessness |
Identify unworkable behavior: behavior that is not moving towards the participant’s values. Identify that control is not the solution but the problem.
|
Meeting each other. Exercise: dealing with unpleasant experiences; the costs of avoidance worksheet* Metaphor: the unwelcome party guest (Aunt Ida) & The monster and the ravine Poem by Mary Oliver; the journey# |
Exercise: dealing with unpleasant experiences. Exercise: Chinese finger trap. Put the drawing of the monster and the ravine on your fridge. Reading handout; handling your homework. Reading; introduction, Chapters 1 and 2 of The Happiness Trap |
|
2 |
Acceptance, Willingness & Contact with the here and now |
Identify that control is not the solution but the problem. Exploring the willingness to face your own fears, emotional pain, negative thoughts. Introduction the human condition. Introduction to mindfulness. |
Discussing homework, including Metaphor: The monster and the ravine Discussing acceptance: the difference between pain and contaminated pain/pain and suffering*. Eating with awareness (the raisin-exercise#), including inquiry. Sitting meditation with attention on breathing, noises and thoughts. |
Doing a daily activity, such as brushing your teeth or having a shower with awareness and full engagement with all the five senses. Reading handout; mindfulness* Reading Chapters 3, 10, 11 and 12 of The Happiness Trap |
|
3 |
Contact with the here and now & Values |
Bringing full awareness to your here and now experiences Introduction to values; clarifying what is most important, significant and meaningful. |
Discussing homework Education about values and the difference with goals. Filling in the Value Questionnaire * and the Actually-questionnaire*. Story; The king who had three sons# |
Doing another daily activity, such as brushing your teeth or having a shower with awareness and full engagement with all the five senses. Reading Chapters 24 and 25 of The Happiness Trap. Filling in the Bull’s Eye (Chapter 25). Which value(s) needs more attention in our life? |
|
4 |
Values & Defusion |
Learning to perceive thoughts, images and other cognitions as what they are: nothing more than bits of language, words and pictures instead of rules and facts. |
Discussing homework with attention on fusion. Teaching about the power of language and doing defusion exercises; thinking about a Napoleon boiled sweet. Introducing the mind of the therapist. |
Practice at home with defusion and inventing a name for your mind. Reading Chapters 4, 5 and 6 of The Happiness Trap. |
|
5 |
Defusion & Contact with the Here and Now |
See session 4 and bringing full awareness to your here and now experiences
|
Discussing homework and experiences with defusion at home. The participants introduce their mind. Metaphors: your mind as storyteller and staying behind the waterfall. Body scan exercise, inquiry and teaching. |
Doing the body scan exercise* 3 times a week Reading Chapters 7, 8, 9, 10 of The Happiness Trap.
|
|
6 |
Self as Context
|
Taking perspective and assessing a transcendent sense of self; a continuity of consciousness that is ever present, unchanging and impervious to harm. |
Discussing homework with attention for obstacles during mindfulness. Introducing the observing self during a mindfulness exercise Exercise; experiencing the observing self Metaphors; chessboard and sky |
Re-evaluation of values using your Value Questionnaire or Bull’s Eye. Exercises*: with yourself through time, I am, Rules versus reality Reading handout: affair “stroopwafel” * (about changing the perspective). Reading Chapters 15, 16, 17 of The Happiness Trap. |
|
7 |
Values |
Further clarifying values; towards a rich, meaningful life; life from your heart and not your mind.
|
Discussing homework: What would you do if you had no fears or doubts? What would you do with 50 million? Participants discuss their personal values, with attention for fusion and willingness to experience unpleasant feelings. |
Reading Chapters 26, 27 and 30 of The Happiness Trap. Making an action plan for one of your values with the goalsetting worksheet in Chapter 27.
|
|
8 |
Commitment: Action and evaluation |
Setting goals guided by your values and taking action to achieve them. |
Discussing homework and formulating committed actions. Evaluating and discussing personal focus of the six core processes in the future Goodbye and final meditation. |
|
*Exercises and handouts are available in Dutch (Link); #poem, story and exercise in Dutch, translation of Segal MBCT protocol.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 13, May 2020Accepted: Tue 02, Jun 2020
Published: Fri 05, Jun 2020
Copyright
© 2023 Ieke Winkens. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2020.02.13
Author Info
Caroline van Heugten Ieke Winkens Iris de Marez Oyens Nicole Geschwind Yvonne Bol
Corresponding Author
Ieke WinkensDepartment of Neuropsychology & Psychopharmacology, Faculty of Psychology and Neuroscience, Maastricht University, Maastricht, The Netherlands
Figures & Tables
Table 1: Participant characteristics.
|
Participant |
Sex |
Age |
Type MS |
Disease duration in years |
EDSS |
SDMT* |
PASAT* |
COWAT* |
CIS-20 |
HADS -D |
HADS- A |
Comorbity |
|
A |
f |
55 |
RRMS |
3 |
1.5 |
0.5 |
-0.1 |
-0.6 |
44 |
14 |
12 |
Migraine |
|
B |
f |
39 |
RRMS |
3 |
1 |
-0.5 |
-0.5 |
-0.5 |
37 |
13 |
16 |
Diabetes mellitus type I |
|
C |
f |
53 |
RRMS |
6 |
2.5 |
-1.5 |
-1.0 |
-1.7 |
51 |
12 |
15 |
Neuropathic pain |
|
D |
f |
58 |
SPMS |
9 |
6.5 |
-0.3 |
-0.6 |
-1.2 |
47 |
8 |
12 |
Hyperhidrosis and ulcerative colitis |
|
E |
f |
41 |
RRMS |
11 |
4 |
0 |
-0.6 |
-0.9 |
48 |
13 |
16 |
- |
|
F |
f |
50 |
RRMS |
3 |
3.5 |
0.7 |
1.3 |
-0.6 |
49 |
7 |
14 |
- |
*: z-scores
MS: Multiple Sclerosis; SPMS: Secondary Progressive Multiple Sclerosis; RRMS: Relapsing Remitting Multiple Sclerosis; EDSS: Expanded Disability Status Scale; SDMT: Symbol Digit Modalities Test; PASAT: Paced Auditory Serial Addition Test; COWAT: Controlled Oral Word Association Test; CIS-20: subscale fatigue of Checklist Individual Strength-20; HADS-D: subscale depression of the Hospital Anxiety and Depression Scale; HADS-A: subscale anxiety of Hospital Anxiety and Depression Scale.
Table 2: Participants’ baseline and post-treatment scores and randomization test results.
|
Visual Analogue Scale – Quality of Life |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
4.63 (1.35) |
5.63* (1.13) |
0.168 |
0.016** |
10 |
|
B |
5.46 (1.10) |
5.75 (0.54) |
0.417 |
0.019** |
12 |
|
C |
4.14 (0.70) |
4.56* (0.62) |
0.012** |
|
|
|
D |
5.79 (0.75) |
6.89* (0.80) |
0.179 |
0.034** |
22 |
|
E |
5.91 (0.75) |
5.93 (0.55) |
0.762 |
|
|
|
F |
6.37 (1.42 ) |
6.25 (1.26) |
0.917 |
|
|
|
Numerical Rating Score – Quality of Life |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
5.67 (0.89) |
6.66* (0.89) |
0.016** |
|
|
|
B |
6.37 (1.10) |
6.56 (0.71) |
0.476 |
0.010** |
11 |
|
C |
4.25 (0.70) |
4.82* (0.62) |
0.042** |
|
|
|
D |
6.11 (0.74) |
6.99* (0.82) |
0.171 |
0.009** |
9 |
|
E |
5.76 (0.68) |
5.81 (0.40) |
0.566 |
|
|
|
F |
6.59 (1.31) |
6.90 (1.45) |
0.685 |
0.036** |
28 |
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Frequencies |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
12.67 (2.52 ) |
15.57* (2.42) |
0.111 |
|
|
|
B |
14.00 (0.89) |
14.36 (1.55) |
1.000 |
|
|
|
C |
8.56 (1.24) |
7.52 (1.17) |
0.750 |
|
|
|
D |
6.33 (2.89) |
11.40* (4.21) |
0.176 |
|
|
|
E |
11.50 (1.64) |
11.00 (1.45) |
0.200 |
|
|
|
F |
13.11 (1.05) |
11.19 (1.44) |
1.000 |
|
|
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Restrictions |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
51.11 (10.18) |
57.50* (4.57) |
0.063 |
|
|
|
B |
75.00 (5.48) |
79.88 (2.81) |
0.276 |
|
|
|
C |
54.44 (5.27) |
56.51 (5.72) |
0.923 |
0.048** |
42 |
|
D |
46.67 (8.82) |
51.57* (18.58) |
0.126 |
|
|
|
E |
54.44 (1.72) |
54.17 (1.48) |
0.357 |
|
|
|
F |
62.96 (4.84) |
66.98 (1.45) |
0.048** |
|
|
|
Utrecht Scale for Evaluation of Rehabilitation - Participation Satisfaction |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
35.83 (3.82) |
52.50* (7.12) |
0.056 |
|
|
|
B |
45.83 (5.63) |
50.71* (6.89) |
1.133 |
|
|
|
C |
48.19 (3.91) |
47.38 (1.24) |
0.583 |
|
|
|
D |
30.00 (8.66) |
59.94* (17.38) |
0.176 |
|
|
|
E |
42.50 (0.00) |
43.25 (1.18) |
0.900 |
0.050** |
105 |
|
F |
51.11 (1.32) |
58.93* (9.44) |
0.750 |
0.042** |
77 |
|
Acceptance & Action Questionnaire II |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
37.25 (4.66) |
43.35* (2.63) |
0.056 |
|
|
|
B |
40.83 (2.11) |
39.00 (4.12) |
0.867 |
|
|
|
C |
43.22 (1.99) |
41.00 (2.27) |
0.750 |
|
|
|
D |
47.67 (4.78) |
64.00* (2.95) |
0.176 |
|
|
|
E |
54.83 (2.85) |
54.45 (2.62) |
0.950 |
|
|
|
F |
37.89 (4.23) |
47.76* (7.83) |
0.667 |
0.042** |
35 |
|
Cognitive Fusion Questionnaire 13 |
|||||
|
Participant |
Baseline Mean (SD) |
Intervention + FU Mean (SD) |
Immediate effect p-values |
Delayed effect p-values |
Number of days until delayed effect reached significance |
|
A |
43.00 (2.92) |
51.05* (3.94) |
0.056 |
|
|
|
B |
50.83 (4.22) |
51.29 (1.98) |
0.733 |
|
|
|
C |
55.44 (3.83) |
54.81 (3.36) |
0.750 |
|
|
|
D |
65.33 (5.73) |
85.55* (4.77) |
0.176 |
|
|
|
E |
67.00 (2.31) |
66.70 (3.07) |
0.850 |
0.050** |
105 |
|
F |
47.11 (2.13) |
62.48* (8.20) |
0.375 |
0.042** |
21 |
*: more than 10% increase from baseline; **: statistically significant increase (p≤0.05); FU: follow-up period; SD: standard deviation.
Appendix Table 1: ACT group protocol: Contents per session.
|
Session |
Core process |
Goal |
During session |
Homework |
|
1 |
Experiental avoidance & Creative hopelessness |
Identify unworkable behavior: behavior that is not moving towards the participant’s values. Identify that control is not the solution but the problem.
|
Meeting each other. Exercise: dealing with unpleasant experiences; the costs of avoidance worksheet* Metaphor: the unwelcome party guest (Aunt Ida) & The monster and the ravine Poem by Mary Oliver; the journey# |
Exercise: dealing with unpleasant experiences. Exercise: Chinese finger trap. Put the drawing of the monster and the ravine on your fridge. Reading handout; handling your homework. Reading; introduction, Chapters 1 and 2 of The Happiness Trap |
|
2 |
Acceptance, Willingness & Contact with the here and now |
Identify that control is not the solution but the problem. Exploring the willingness to face your own fears, emotional pain, negative thoughts. Introduction the human condition. Introduction to mindfulness. |
Discussing homework, including Metaphor: The monster and the ravine Discussing acceptance: the difference between pain and contaminated pain/pain and suffering*. Eating with awareness (the raisin-exercise#), including inquiry. Sitting meditation with attention on breathing, noises and thoughts. |
Doing a daily activity, such as brushing your teeth or having a shower with awareness and full engagement with all the five senses. Reading handout; mindfulness* Reading Chapters 3, 10, 11 and 12 of The Happiness Trap |
|
3 |
Contact with the here and now & Values |
Bringing full awareness to your here and now experiences Introduction to values; clarifying what is most important, significant and meaningful. |
Discussing homework Education about values and the difference with goals. Filling in the Value Questionnaire * and the Actually-questionnaire*. Story; The king who had three sons# |
Doing another daily activity, such as brushing your teeth or having a shower with awareness and full engagement with all the five senses. Reading Chapters 24 and 25 of The Happiness Trap. Filling in the Bull’s Eye (Chapter 25). Which value(s) needs more attention in our life? |
|
4 |
Values & Defusion |
Learning to perceive thoughts, images and other cognitions as what they are: nothing more than bits of language, words and pictures instead of rules and facts. |
Discussing homework with attention on fusion. Teaching about the power of language and doing defusion exercises; thinking about a Napoleon boiled sweet. Introducing the mind of the therapist. |
Practice at home with defusion and inventing a name for your mind. Reading Chapters 4, 5 and 6 of The Happiness Trap. |
|
5 |
Defusion & Contact with the Here and Now |
See session 4 and bringing full awareness to your here and now experiences
|
Discussing homework and experiences with defusion at home. The participants introduce their mind. Metaphors: your mind as storyteller and staying behind the waterfall. Body scan exercise, inquiry and teaching. |
Doing the body scan exercise* 3 times a week Reading Chapters 7, 8, 9, 10 of The Happiness Trap.
|
|
6 |
Self as Context
|
Taking perspective and assessing a transcendent sense of self; a continuity of consciousness that is ever present, unchanging and impervious to harm. |
Discussing homework with attention for obstacles during mindfulness. Introducing the observing self during a mindfulness exercise Exercise; experiencing the observing self Metaphors; chessboard and sky |
Re-evaluation of values using your Value Questionnaire or Bull’s Eye. Exercises*: with yourself through time, I am, Rules versus reality Reading handout: affair “stroopwafel” * (about changing the perspective). Reading Chapters 15, 16, 17 of The Happiness Trap. |
|
7 |
Values |
Further clarifying values; towards a rich, meaningful life; life from your heart and not your mind.
|
Discussing homework: What would you do if you had no fears or doubts? What would you do with 50 million? Participants discuss their personal values, with attention for fusion and willingness to experience unpleasant feelings. |
Reading Chapters 26, 27 and 30 of The Happiness Trap. Making an action plan for one of your values with the goalsetting worksheet in Chapter 27.
|
|
8 |
Commitment: Action and evaluation |
Setting goals guided by your values and taking action to achieve them. |
Discussing homework and formulating committed actions. Evaluating and discussing personal focus of the six core processes in the future Goodbye and final meditation. |
|
*Exercises and handouts are available in Dutch (Link); #poem, story and exercise in Dutch, translation of Segal MBCT protocol.
References
- Compston A, Coles A (2008) Multiple Sclerosis. Lancet 372: 1502-1517. [Crossref]
- Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M et al. (2015) The Incidence and Prevalence of Psychiatric Disorders in Multiple Sclerosis: A Systematic Review. Mult Scler 21: 305-317. [Crossref]
- Johansson S, Ytterberg C, Claesson IM, Lindberg J, Hillert J et al. (2007) High Concurrent Presence of Disability in Multiple Sclerosis. Associations With Perceived Health. J Neurol 254: 767-773. [Crossref]
- Mitchell AJ, Benito León J, González JMM, Rivera Navarro J (2005) Quality of Life and Its Assessment in Multiple Sclerosis: Integrating Physical and Psychological Components of Wellbeing. Lancet Neurol 4: 556-566. [Crossref]
- Possa MF , Minacapelli E, Canale S, Comi G, Martinelli V et al. (2017) The First Year After Diagnosis: Psychological Impact on People With Multiple Sclerosis. Psychol Health Med 22: 1063-1071. [Crossref]
- Brenner P,Piehl F (2016) Fatigue and Depression in Multiple Sclerosis: Pharmacological and Non-Pharmacological Interventions. Acta Neurol Scand 134: 47-54. [Crossref]
- Thomas PW, Thomas S, Hillier C, Galvin K, Baker R (2006) Psychological Interventions for Multiple Sclerosis. Cochrane Database Syst Rev CD004431. [Crossref]
- Calandri E, Graziano F, Borghi M, Bonino S (2017) Improving the Quality of Life and Psychological Well-Being of Recently Diagnosed Multiple Sclerosis Patients: Preliminary Evaluation of a Group-Based Cognitive Behavioral Intervention. Disabil Rehabil 39: 1474-1481. [Crossref]
- Dennison L, Moss Morris R, Chalder T (2009) A Review of Psychological Correlates of Adjustment in Patients With Multiple Sclerosis. Clin Psychol Rev 29 141-153. [Crossref]
- Borghi M, Bonino S, Graziano F, Calandri E (2018) Exploring Change in a Group-Based Psychological Intervention for Multiple Sclerosis Patients. Disabil Rehabil 40: 1671-1678. [Crossref]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J (2006) Acceptance and Commitment Therapy: Model, Processes and Outcomes. Behav Res Ther 44: 1-25. [Crossref]
- Arch JJ, Mitchell JL (2015) An Acceptance and Commitment Therapy (ACT) Group Intervention for Cancer Survivors Experiencing Anxiety at Re-Entry. Psychooncology 25: 610-615. [Crossref]
- Twohig MP, Levin ME (2017) Acceptance and Commitment Therapy as a Treatment for Anxiety and Depression: A Review. Psychiatr Clin North Am 40: 751-770. [Crossref]
- Buhrman M, Skoglund A, Husell J, Bergström K, Gordh T et al. (2013) Guided Internet-Delivered Acceptance and Commitment Therapy for Chronic Pain Patients: A Randomized Controlled Trial. Behav Res Ther 51: 307-315. [Crossref]
- A Tjak JGL, Davis ML, Morina N, Powers MB, Smits JAJ et al. (2015) A Meta-Analysis of the Efficacy of Acceptance and Commitment Therapy for Clinically Relevant Mental and Physical Health Problems. Psychother Psychosom 84: 30-36. [Crossref]
- Pakenham KI (1999) Adjustment to Multiple Sclerosis: Application of a Stress and Coping Model. Health Psychol 18: 383-392. [Crossref]
- Veehof MM, Oskam MJ, Schreurs KMG, Bohlmeijer ET (2011) Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain 152: 533-542. [Crossref]
- Sheppard SC, Forsyth JP, Hickling EJ, Bianchi J (2010) A Novel Application of Acceptance and Commitment Therapy for Psychosocial Problems Associated with Multiple Sclerosis. Int J MS Care 12: 200-206.
- Nordin L, Rorsman I (2012) Cognitive Behavioural Therapy in Multiple Sclerosis: A Randomized Controlled Pilot Study of Acceptance and Commitment Therapy. J Rehabil Med 44: 87-90. [Crossref]
- Harrison AM, McCracken LM, Jones K, Norton S, Moss Morris R (2016) Using Mixed Methods Case-Series Evaluation in the Development of a Guided Self-Management Hybrid CBT and ACT Intervention for Multiple Sclerosis Pain. Disabil Rehabil 39: 1785-1798. [Crossref]
- Amir F, Ahadi H, Nikkhah K, Seirafi M (2017) The Effectiveness of Acceptance and Commitment Group Therapy and Group Logotherapy in Reducing Perceived Stress among MS Patients. Caspian J Neurol Sci 3: 175-184.
- Bayati A, Abbasi P, Bashiri H, Dehghan F, Yazdanbakhsh K (2017) The Effectiveness of Acceptance and Commitment Therapy on Psychological Well-Being in Women with Ms. Iioab Journal 8: 82-86.
- Proctor BJ, Moghaddam NG, Evangelou N, Das Nair R (2018) Telephone-supported acceptance and commitment bibliotherapy for people with multiple sclerosis and psychological distress: A pilot randomised controlled trial. J Context Behav Sci 9: 103-109.
- Pakenham K I, Mawdsley M, Brown FL, Burton NW (2018) Pilot Evaluation of a Resilience Training Program for People With Multiple Sclerosis. Rehabil Psychol 63: 29-42. [Crossref]
- Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA et al. (2011) Diagnostic Criteria for Multiple Sclerosis: 2010 Revisions to the McDonald Criteria. Ann Neurol 69: 292-302. [Crossref]
- Post MWM, van der Zee CH, Hennink J, Schafrat CG, Visser Meily JMA et al. (2012) Validity of the Utrecht Scale for Evaluation of Rehabilitation-Participation. Disabil Rehabil 34: 478-485. [Crossref]
- Kurtzke JF (1983) Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 33: 1444-1452. [Crossref]
- Benedict RHB, Fischer JS, Archibald CJ, Arnett PW, Beatty WW et al. (2002) Minimal Neuropsychological Assessment of MS Patients: A Consensus Approach. Clin Neuropsychol 16: 381-397. [Crossref]
- Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67: 361-370. [Crossref]
- Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE et al. (1997) A Validation Study of the Hospital Anxiety and Depression Scale (HADS) in Different Groups of Dutch Subjects. Psychol Med 27: 363-370. [Crossref]
- Honarmand K, Feinstein A (2009) Validation of the Hospital Anxiety and Depression Scale for Use With Multiple Sclerosis Patients. Mult Scler 15: 1518-1524. [Crossref]
- Vercoulen JHMM, Alberts M, Bleijenberg G (1999) De checklist individuele spankracht (CIS). Gedragstherapie 32: 131-136.
- Worm Smeitink M, Gielissen M, Bloot L, Van Laarhoven HWM, Van Engelen BGM et al. (2017) The Assessment of Fatigue: Psychometric Qualities and Norms for the Checklist Individual Strength. J Psychosom Res 98: 40-46. [Crossref]
- Dittner AJ, Wessely SC, Brown RG (2004) The Assessment of Fatigue: A Practical Guide for Clinicians and Researchers. J Psychosom Res 56: 157-170. [Crossref]
- Arruda JE, Stern RA, Legendre SA (1996) Assessment of Mood State in Patients Undergoing Electroconvulsive Therapy: The Utility of Visual Analog Mood Scales Developed for Cognitively Impaired Patients. Convuls Ther 12: 207-212. [Crossref]
- Price DD, McGrath PA, Rafii A, Buckingham B (1983) The Validation of Visual Analogue Scales as Ratio Scale Measures for Chronic and Experimental Pain. Pain 17: 45-56. [Crossref]
- De Boer AGEM, van Lanschot JJB, Stalmeier PFM, van Sandick JW, Hulscher JBF et al. (2004) Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res 13: 311-320. [Crossref]
- Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW et al. (2011) Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage 41: 1073-1093. [Crossref]
- Phan NQ, Blome C, Fritz F, Gers, J, Reich A et al. (2012) Assessment of Pruritus Intensity: Prospective Study on Validity and Reliability of the Visual Analogue Scale, Numerical Rating Scale and Verbal Rating Scale in 471 Patients With Chronic Pruritus. Acta Derm Venereol 92: 502-507. [Crossref]
- Price DD, Bush FM, Long S, Harkins SW (1994) A Comparison of Pain Measurement Characteristics of Mechanical Visual Analogue and Simple Numerical Rating Scales. Pain 56: 217-226. [Crossref]
- Jacobs J, Kleen M, De Groot F, A Tjak J (2008) Het meten van experiëntiële vermijding. De Nederlandstalige versie van de Acceptance and Action Questionnaire-II: The measurement of experiential avoidance. The Dutch language version of the Acceptance and Action Questionnaire-II (AAQ-II). Gedragstherapie 4: 349-364.
- Fledderus M, Bohlmeijer ET, Fox JP, Schreurs KMG, Spinhoven P (2013) The Role of Psychological Flexibility in a Self-Help Acceptance and Commitment Therapy Intervention for Psychological Distress in a Randomized Controlled Trial. Behav Res Ther 51: 142-151. [Crossref]
- Gillanders D, Bolderston H, Bond F (2011) Cognitive Fusion Questionnaire. Assoc Context Behav Sci.
- Gillanders DT, Bolderston H, Bond FW, Dempster M, Flaxman PE et al. (2014) The Development and Initial Validation of the Cognitive Fusion Questionnaire. Behav Ther 45: 83-101. [Crossref]
- Jansen G, Batink T (2014) Time to ACT. Thema, Uitgeverij van Schouten en Nelissen Zaltbommel.
- Luoma JB, Hayes SC, Walser RD (2007) Learning ACT: An Acceptance & Commitment Therapy Skills-Training Manual for Therapists. Context Press Oakland, CA.
- Harris R (2012) De valstruik van het geluk. Hoe kun je stoppen met worstelen en beginnen met leven. Bohn Stafleu van Loghum Houten.
- Bulté I, Onghena P (2012) When the Truth Hits You Between the Eyes. Methodology 8: 104-114.
- Perdices M, Tate RL (2009) Single-subject Designs as a Tool for Evidence-Based Clinical Practice: Are They Unrecognised and Undervalued? Neuropsychol Rehabil 19: 904-927. [Crossref]
- Ter Kuile MM, Bulté I, Weijenborg PTM, Beekman A, Melles R et al. (2009) Therapist-aided Exposure for Women With Lifelong Vaginismus: A Replicated Single-Case Design. J Consult Clin Psychol 77: 149-159. [Crossref]
- Grossman P, Kappos L, Gensicke H, D’Souza M, Mohr DC et al. (2010) MS Quality of Life, Depression, and Fatigue Improve After Mindfulness Training: A Randomized Trial. Neurology 75: 1141-1149. [Crossref]
- Hind D, Cotter J, Thake A, Bradburn M, Cooper C et al. (2014) Cognitive Behavioural Therapy for the Treatment of Depression in People With Multiple Sclerosis: A Systematic Review and Meta-Analysis. BMC Psychiatry 14: 5. [Crossref]
- Bulté I, Onghena P (2009) Randomization tests for multiple-baseline designs: an extension of the SCRT-R package. Behav Res Methods 41: 477-485. [Crossref]
- Kazdin AE, Kopel SA (1975) On resolving ambiguities of the multiple-baseline design: Problems and recommendations. Behav Ther 6: 601-608.
- Vilardaga R, Bricker J, McDonell M (2014) The Promise of Mobile Technologies and Single Case Designs for the Study of Individuals in Their Natural Environment. J Contextual Behav Sci 3: 148-153. [Crossref]
- Kazdin AE (2007) Mediators and Mechanisms of Change in Psychotherapy Research. Annu Rev Clin Psychol 3: 1-27. [Crossref]
- Swain J, Hancock K, Hainsworth C, Bowman J (2014) Mechanisms of change: Exploratory outcomes from a randomised controlled trial of acceptance and commitment therapy for anxious adolescents. J Context Behav Sci 4: 56-67.
- Wicksell RK, Olsson GL, Hayes SC (2010) Psychological flexibility as a mediator of improvement in Acceptance and Commitment Therapy for patients with chronic pain following whiplash. Eur J Pain 14: 1059.e1-1059.e11. [Crossref]

