Journals
The Clinical Significance of L5 Incidence in Patients with High Pelvic Incidence: A Case Report
A B S T R A C T
Objective: To present a case of sagittal malalignment with high pelvic incidence and its surgical management.
Summary of Background Data: Though rare, patients with high pelvic incidence (PI) around 90° without spondylolisthesis or spondylolysis often show sagittal malalignment with low back pain. However, little has been reported about the treatment of such cases.
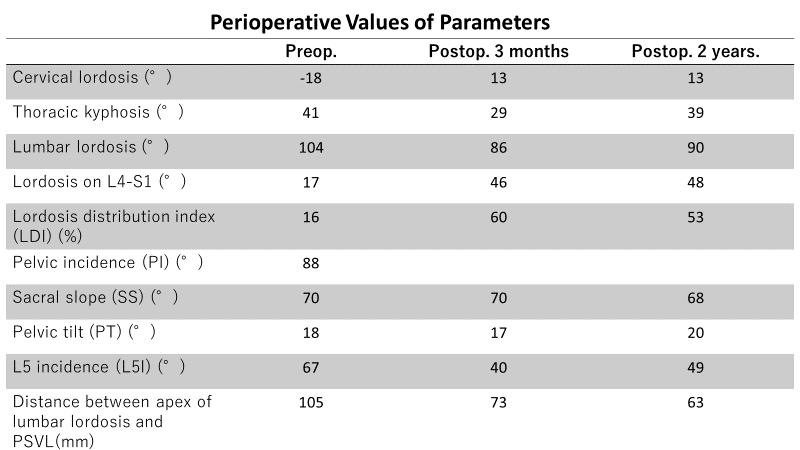
Methods: We report a case of a 15-year-old female complaining of severe difficulty in maintaining an upright position and gait disturbance due to back pain. Radiographs showed high PI of 88° and L5 incidence (L5I) of 67° combined with hyperlordosis of lumbar segments. A lower Lordosis Distribution Index (LDI; percentage of lordosis on segments L4–S1 in entire lumbar lordosis of L1-S1) was detected despite the high overall lumbar lordosis. The patient was surgically treated by two-stage combined posterior and anterior short fusion from the sacrum.
Results: The surgical strategy was planned with attention to L5I instead of PI. L5I decreased to 49° and sagittal alignment of the whole spine—including cervical, thoracic, and lumbar spine—improved without any complications. Activity of daily living (ADL)improved preoperatively with relief of low back pain.
Conclusion: Improvement of L5I by performing short fusion from L4 to S1 may be a strategy for patients with high PI complaining of low back pain due to sagittal malalignment.
Keywords
pelvic incidence, L5 incidence, lower distribution index
Introduction
Pelvic parameters are recognized as one of the keys for evaluating whether patients have sagittal alignment or sagittal malalignment. Schwab et al. reported that a pelvic incidence (PI) minus lumbar lordosis (LL) of 10° or less was the ideal spinopelvic alignment for reducing postoperative pain and disability [1]. Furthermore, Schwab et al. analyzed sagittal malalignment of adult patients with spinal deformity and classified them into four types of curvature with three modifiers: PI-LL, pelvic tilt, and coronal balance. These form the basis of the Scoliosis Research Society–Schwab (SRS-Schwab) adult spinal deformity classification [2]. This classification is now widely used to evaluate postoperative sagittal status in terms of postoperative junctional kyphosis, instrumentation failure, and quality of life.
However, the SRS-Schwab classification cannot solve sagittal malalignment for all types of adult deformity, while some of patients exhibited excellent surgical outcome by making surgical strategy according to SRS-Shwab Classification [Glassman, others]. One limitation of the SRS-Schwab classification is its dependence on the formula “PI-LL.” The average PI in humans ranges from 45° to 55°, although some individuals may have extremely high (≥70°) or low (≤30°) PI without any subjective or objective symptoms [3]. Following the SRS-Schwab classification, a minimum LL of 70° is required in patients with 80° PI. However, it would not be acceptable that patients with extremely high PI be treated to produce extreme lumbar hyperlordosis. Thus, alternative concepts and approaches are required for treating patients with high PI.
Bodin, et al. introduced a treatment method of changing the magnitude of PI in each patient using sacral or pelvic osteotomy to adopt a “PI-LL ≤ 10°” concept [4]. In other words, this approach puts patients with high PI closer to those with typical PI and thus makes it possible to treat them using standard concepts. However, this is a new approach. As only a small number of patients have been treated by pelvic osteotomy, it is too early to discuss its clinical outcome. On the other hand, L5 incidence (L5I) is another parameter often used for spondylolisthesis instead of PI. As high-grade spondylolisthesis is usually due to a dome-shaped S1 plateau, which makes measuring of PI difficult, L5I is a useful indicator in surgical treatment. Furthermore, L5I may be applicable when considering surgical treatment of patients with high PI because high-grade spondylolisthesis quite often has high PI. This case report presents the surgical effect of L4–S1 fusion with attention to L5I, not PI, for a patient with high PI.
Case Overview
A 14-year-old female visited our clinic after referral through a school screening program. She had slight scoliosis of 20° with hyperlordosis of the lumbar area. She also complained of back pain and gait disturbance. She had no abnormal medical history except for frequent episodes of enuresis until the age of 11. There was no family history of musculoskeletal-related disorders.
I Physically examination at age 14
The patient had a height of 138 cm and body weight of 33 kg. Her trunk–limb proportion was reminiscent of limb shortening, and she kept a standing posture with her buttocks protruded posteriorly and bilateral knees and hips slightly flexed. Lumbar extension worsened low back pain without any radiation pain to the lower extremities. A straight leg raise test was bilaterally negative. She had no neurological deficits. Range of motion of bilateral hips and knees did not show any abnormal limitations.
Figure 1: Preoperative plain radiographic images. The patient had scoliosis of 20° and sagittal malalignment showing longer lordotic segments with hyperlordosis of 104°. Note that the sacrum is angular shaped with extremely high PI (88°).
II Radiographic evaluation
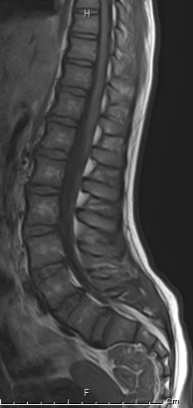
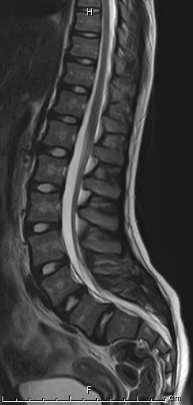
An anteroposterior radiographic image in an erect position showed 20° scoliosis. Preoperative sagittal parameters are shown in (Table 1). A plain lateral radiographic image in an upright position showed severe hyperlordosis with longer segments of lordosis and the inflexion point of T9 (Figure 1). It also demonstrated an angular-shaped sacrum with sharp sacral tilt. Magnetic resonance imaging did not show any abnormalities (Figure 2).
Figure 2: Preoperative MRI. No abnormalities were detected in MRI, except hyperlordosis of lumbar segments.
Figure 3: Plain radiographic images taken 2 years postoperatively. Scoliosis was spontaneously corrected. Sagittal malalignment improved showing L5I of 64° and a decrease of lordotic segments with inflexion point at T11. The sagittal plain radiographic image showed straight hip and knee joints postoperatively, which had been slightly flexed in an upright position preoperatively.
III Surgical Intervention
To increase lordosis on distal lumbar segments on L4-S1 (equal to a decrease of L5I), we planned and performed two-staged correction and fusion from L4 to the sacrum. In the first operation, posterior lumber fusion was performed using pedicle screws. We tried to obtain maximum lordosis between L4 and S1 as long as possible by posterior compression following Smith–Petersen osteotomy at L4/5 and L5/S. One week after the first surgery, anterior lumbar fusion was performed at L4/5 and L5/S1 with expandable interbody cages and morselized bone graft via a left pararectal approach. There were no intraoperative or postoperative complications in both surgeries.
Table 1
IV Postoperative Course
Postoperative immobilization was achieved using a Spica-brace for 3 months. The patient gradually regained walking ability through a physical rehabilitation program with relief of low back pain. Postoperative sagittal parameters are shown in (Table 1). The inflexion point of sagittal curvature changed from T9 to T11. At two years postoperative, fusion was achieved through the radiography images and no loosening of cages and screws was detected (Figure 3). The patient reported no difficulty in walking and no back pain at the 2-year postoperative follow-up.
Discussion
Duval-Beaupère et al. reported that PI is consistent for each individual and is thus the key factor to determine LL for managing spinal balance [5]. The mean value of PI in adult humans is approximately 50°, although there are slight differences among races. Definitions of low PI and high PI have not been determined, however, values below 35° and above 85°, respectively are commonly used. Roussouly et al. proposed a classification by dividing sagittal alignment into four types according to the values of PI and SS with attention to the inflexion point, which is a transition segment from the thoracic kyphosis to LL [6]. They emphasized that it is of great importance to separate patients with low PI or high PI from those with normal PI when planning surgical treatment of adult spinal deformities. However, no consensus related to surgical strategy in patients with extremely low or high PI has been reached because of the relatively small number of such patients. Furthermore, it has not been determined how low PI and high PI affect long-term activities of daily living. Bodin et al. described two surgical approaches to decrease the magnitude of PI in patients with high PI: sacral osteotomy and pelvic osteotomy [4]. Both approaches are effective in theory; however, they may not be standard treatments because of difficulty in determining the ideal angle of osteotomy during surgery and stabilizing the osteotomized segments until solid bone union is achieved, even when using metal implants.
Hresko et al. reported that the mean value of L5I in asymptomatic populations with high PI over 70° is 38.3 ± 7.0° [7]. Barrey et al. noted that 2/3 of LL is located in the lower lumbar segments between L4 and S1 [8]. In a recent study, Yilgor et al. proposed a Global Alignment and Proportion Score for the evaluation of surgical effect in patients with adult spinal deformities [9]. They adopted a Lordosis Distribution Index (LDI) by dividing the value of L4–S1 lordosis by L1–S1 lordosis, where 50–80% is defined as the ideal index. In the present case, L5I was extremely high and LDI was quite low despite high lordosis of the longer lordosis segments. The surgical procedure we performed achieved LDI of 60% and 53% at postoperative periods of 3 months and 2 years, respectively. These LDI values are very close to the ideal value in normal populations. The surgical intervention achieved reduction of L5I without any surgical complications, in spite of slight loss of correction. As a result, lumbar and whole sagittal alignment in an erect position improved because of caudal movement of the inflexion point from T9 to T11, followed by an overall decrease in LL. However, LL did not reach normal values, and long-term follow-up is recommended.
Conclusion
We reported a case of high PI surgically treated by short fusion from L4 to S1 to decrease L5I, instead of PI, and increase the LDI. This approach may be an alternative for treatment of patients with high PI complaining of sagittal malalignment and low back pain.
Article Info
Article Type
Case ReportPublication history
Received: Sat 08, Jun 2019Accepted: Sat 29, Jun 2019
Published: Sat 06, Jul 2019
Copyright
© 2023 Ippei Yamauchi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.04.01
Author Info
Ippei Yamauchi Noriaki Kawakami Ryoji Tauchi Tetsuya Ohara Toshiki Saito
Corresponding Author
Ippei YamauchiDepartment of Orthopaedics and Spine Surgery, Meijo Hospital
Figures & Tables




References
- Schwab F, Patel A, Ungar B, Farcy J, Lafage V (2010) Adult Spinal Deformity-Postoperative Standing Imbalance: How Much Can You Tolerate? An Overview of Key Parameters in Assessing Alignment and Planning Corrective Surgery. Spine 35: 2224-2231. [Crossref]
- Schwab F, Ungar B, Blondel B, Buchowski J, Coe J et al. (2012) Scoliosis Research Society-Schwab Adult Spinal Deformity Classification: A Validation Study. Spine 37: 1077-1082. [Crossref]
- Tardieu C, Hasegawa K, Haeusler M (2017) How Did the Pelvis and Vertebral Column Become a Functional Unit during the Transition from Occasional to Permanent Bipedalism? Anat Rec (Hoboken) 300: 912-931. [Crossref]
- Bodin A, Roussouly P (2015) Sacral and pelvic osteotomies for correction of spinal deformities. Eur Spine J 24: S72S-82. [Crossref]
- Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7: 99-103. [Crossref]
- Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the Normal Variation in the Sagittal Alignment of the Human Lumbar Spine and Pelvis in the Standing Position. Spine 30: 346-353. [Crossref]
- Hresko MT, Labelle H, Roussouly P, Berthonnaud E (2007) Classification of High-Grade Spondylolistheses Based on Pelvic Version and Spine Balance. Spine 32: 2208-2213. [Crossref]
- Barrey C, Darnis A (2015) Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop 6: 117-126. [Crossref]
- Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I et al. (2017) Global Alignment and Proportion (GAP) Score Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J Bone Joint Surg Am 99: 1661-1672. [Crossref]
