Surgical Management of Disseminated Pulmonary Mucormycosis in the Immunocompromised
A B S T R A C T
Background: Pulmonary mucormycosis is a rare and aggressive fungal infection that is known to predominantly affect immunocompromised hosts. Early surgical resection with prolonged antimycotic therapy is an established therapy for localized disease; however, the role of surgery in multifocal pulmonary disease is less clear.
Case: We report successful treatment of medically refractory disseminated pulmonary mucormycosis with a salvage lobectomy and intrapleural antibiosis in a 58-year-old immunocompromised female.
Conclusion: Surgery resection of necrotic foci in disseminated pulmonary mucormycosis is a viable surgical treatment option even if extensive resection is required. This treatment option should be considered early, given the high incidence of medically refractory disease.
Keywords
Mucormycosis, pulmonary, immunocompromised, lobectomy, lesection
Introduction
Mucormycosis is an opportunistic infection with an estimated incidence of 1.7 cases per million people per year in the United States. Immunocompromised patients are particularly vulnerable to this pathogen and represent the vast majority of those afflicted with it. Pulmonary mucormycosis is a distinct clinical entity representing 20% of all cases [1]. The pathogenesis of pulmonary infection is characterized by rapid local progression, angioinvasion, and parenchymal necrosis. For patients who present with anatomically confined disease, early surgical resection with a prolonged antimycotic has been shown to be an effective strategy that is more effective than surgical or medical therapy alone [2-4]. Less is known about the optimal management of those patients with an advanced, multi-lobar disease. We report a case of multifocal pulmonary mucormycosis in a 58-year-old immunocompromised patient successfully treated with surgical resection and intrapleural antibiotic lavage.
Case Report
The patient is a 58-year-old white female who was diagnosed with acute erythroblastic leukemia for which she underwent induction therapy with cytarabine and idarubicin followed by consolidation therapy with High-Dose Cytarabine (HiDAC). Shortly after her final cycle of HiDAC she was admitted with generalized weakness, fatigue, and dyspnea on exertion. On routine laboratory testing, she was found to be profoundly cytopenic with a white blood cell (WBC) count of 0.1 thou/μL, hemoglobin (Hg) of 6.6 g/dL, and undetectable platelets. She was found to have bilateral reticulonodular infiltrates on chest X-ray (CXR) and was subsequently admitted for neutropenic sepsis and pneumonia. She was started on broad-spectrum antibiotics, including vancomycin, cefepime, and azithromycin, in addition to her antifungal prophylaxis with voriconazole. Her respiratory status continued to decline after admission, prompting a chest CT scan, which identified new focal consolidation in the right lower lobe measuring 6 cm x 6 cm x 8 cm with associated extensive diffuse bilateral centrilobular nodular opacities. Her respiratory function continued to decline, and she remained febrile despite broad-spectrum antibiotic and antifungal coverage. Cultures from a transbronchial biopsy of the right lower lobe mass grew pulmonary mucormycosis. The patient was started on liposomal amphotericin B and initially responded to medical treatment but subsequently developed acute respiratory decompensation at day seven of therapy, requiring BiPAP. Repeat chest CT scan imaging showed a progressively enlarging mass in the right lower lobe with cavitation (Figure 1). She was subsequently transferred to our center for thoracic surgical evaluation.
Figures 1: Cross sectional imaging obtained pre-operatively (row 1), one week post operatively (row 2) and 3 months post operatively (row 3). Representative cross-sectional images are shown from coronal cuts (columns A-C) and axial (column D).
After an extensive multidisciplinary review, a decision was made to proceed to with high-risk surgery to resect the necrotic mass in the right lower lobe and it was clear that this process was medically refractory. She was taken to the operating room for a thoracoscopic resection of the right lower lobe. Following placement of standard camera and working ports and a limited mobilization of the right lower lobe it became clear that a minimally invasive approach could not be safely performed. A muscle-sparing thoracotomy was performed, and the right lower lobe was separated from the chest wall. After painstaking dissection of acutely inflamed structures, a standard right lower lobe lobectomy was safely performed. The specimen was sent for permanent histopathologic and microbiologic analysis. Gram stain was unexpectedly positive for gram positive cocci, and as such a 7 French triple lumen pleural catheter was inserted into the seventh intercostal space in anticipation of intrapleural antibiosis. The patient would not wean from the ventilator post operation and required low dose vasopressors and admission to the surgical intensive care unit (SICU).
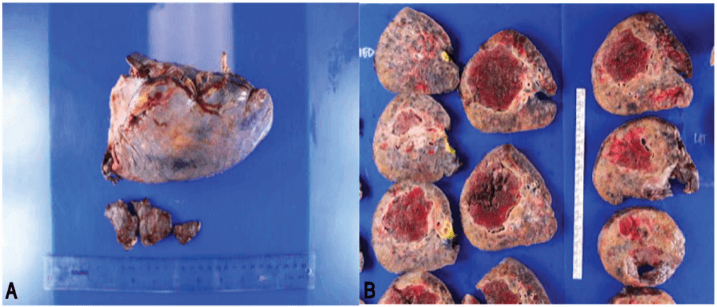
The final pathology of the 10 cm necrotic mass revealed angioinvasive fungal infection consistent with mucormycosis in addition to a bacterial superinfection with vancomycin-resistant enterococcus (VRE) (Figure 2).
Figures 2: A) Gross photograph of the excised right lower lobe. B) Sectioned right lower lobe showing a large (10×8×6) necrotic mass with a fubropurulent rim.
Antibiotic coverage included intrathoracic irrigation with bacitracin in addition to intravenous (IV) linezolid and amphotericin B. She was ultimately extubated on postoperative day (POD) #3 and transferred to the floor on POD #5. Her chest drains were removed on POD #7 and she was discharged home on POD #10 with an extended course of intravenous amphotericin and linezolid. At 2-week follow up, she was found to be recovering well without signs of pulmonary infection and an overall improvement in performance status. Imaging obtained three months post operation similarly demonstrates a complete resolution of her pulmonary disease (Figure 1).
Conclusion
Mucormycosis is an aggressive pathogen that can produce a host of clinical syndromes in immunocompromised hosts. Pulmonary mucormycosis represents a patient subset that tends to affect those with hematologic malignancy and carries with it substantial morbidity and mortality. The prognosis and outcomes of this infection have improved over the last several years as a result of early diagnosis, surgical debridement, and newer antifungal agents. Recommended antifungal treatment includes liposomal amphotericin B, but there are concerns about the limited penetration of antifungals to the affected tissues, due to the presence of necrosis that accompanies this infection. Several studies have shown that the combination of early surgical resection and antifungal therapy has a significant improvement in survival when compared to antifungal therapy alone [5, 6].
Less is known regarding the role of surgery in patients with medically refractory and multifocal disease. We report a case of pulmonary mucormycosis in an immunocompromised host undergoing high dose consolidative chemotherapy for acute erythroblastic leukemia. She was initially managed with liposomal amphotericin B though she exhibited signs of progression and ultimately underwent a salvage lobectomy for medically refractory disease. Postoperatively, the patient was treated with a prolonged course of liposomal amphotericin B to which she responded well. Three months post operation, there was no evidence of recurrent disease and the patent has recovered fully from her operation. Aggressive surgical therapy for multifocal pulmonary mucormycosis is a viable option for advanced disease in carefully selected patients.
Article Info
Article Type
Case ReportPublication history
Received: Wed 08, Apr 2020Accepted: Thu 23, Apr 2020
Published: Thu 30, Apr 2020
Copyright
© 2023 Justin D. Blasberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.04.09
Author Info
Alex Sotolongo Frank Detterbeck Justin D. Blasberg
Corresponding Author
Justin D. BlasbergYale New Haven Hospital, Yale University, Connecticut, USA
Figures & Tables

References
- Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ et al. (2012) Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 54: S23-S34. [Crossref]
- Cornely OA, Arikan Akdagli S, Dannaoui E, Groll AH, Lagrou K et al. (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect 20: 5-26. [Crossref]
- Multani A, Reveron Thornton R, Garvert DW, Gomez CA, Montoya JG et al. (2019) Cut it out! Thoracic surgeon’s approach to pulmonary mucormycosis and the role of surgical resection in survival. Mycoses 62: 893-907. [Crossref]
- Afolayan O, Copeland H, Zaheer S, Wallen JM (2017) Pulmonary Mucormycosis Treated With Lobectomy. Ann Thorac Surg 103: e531-e533. [Crossref]
- Choi H, Lee H, Jeon K, Suh GY, Shin S et al. (2019) Factors affecting surgical resection and treatment outcomes in patients with pulmonary mucormycosis. J Thorac Dis 11: 892-900. [Crossref]
- Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD et al. (1994) Pulmonary mucormycosis: Results of medical and surgical therapy. Ann Thorac Surg 57: 1044-1050. [Crossref]
