Staged Orthodontic, Orthognathic Surgery and Open Septorhinoplasty for Management of Cleidocranial Dysplasia: A Case Report
A B S T R A C T
Background: Cleidocranial dysplasia (CCD) is a rare autosomal dominant disorder with a prevalence of 1:1,000,000. These patients often present with dentofacial deformities such as midface hypoplasia, multiple supernumeraries and delayed eruption and non-eruption of permanent teeth.
Case Presentation: We report a staged orthodontic, orthognathic surgery and open septorhinoplasty management of a 13-year-old male Chinese Singaporean patient diagnosed with cleidocranial dysplasia. He presented with multiple retained primary teeth, buried supernumerary teeth and unerupted permanent teeth. He had a Class III malocclusion and concave facial profile. The multidisciplinary management, which took place over 12 years, resulted in much improved occlusion and facial aesthetics.
Conclusion: Collaboration of different specialties and careful planning is required for the successful treatment of cleidocranial dysplasia.
Keywords
Cleidocranial dysplasia, staged, orthognathic surgery, septorhinoplasty
Background
Cleidocranial dysplasia (CCD) is a rare autosomal dominant disorder with a prevalence of 1:1,000,000. It is characterized by delayed or absent fontanel closure, parietal and frontal bossing, hypoplasia or aplasia of the clavicles, and narrow thorax. Some patients also present with deafness, hypertelorism and low nasal bridge. CCD patients often have maxillary hypoplasia and mandibular prognathism [1]. Dental manifestations include delayed exfoliation of primary teeth, delayed eruption or non-eruption of permanent teeth, supernumerary teeth, retention cysts, and enamel hypoplasia [2].
Case Presentation
A 13-year old Chinese Singaporean boy diagnosed with CCD was seen at the National Dental Centre of Singapore. He was referred by the School Dental Service for management of delayed eruption of his permanent teeth. Clinically he presented with 17 retained primary teeth, Class III malocclusion and a concave facial profile. Radiographic examination revealed 11 buried supernumerary teeth. All his supernumerary teeth were surgically removed under general anaesthesia. Subsequently he had sequential extractions of #53, 54, 63, 64, 73 & 83 (FDI dental notation) to allow for eruption of his permanent teeth.
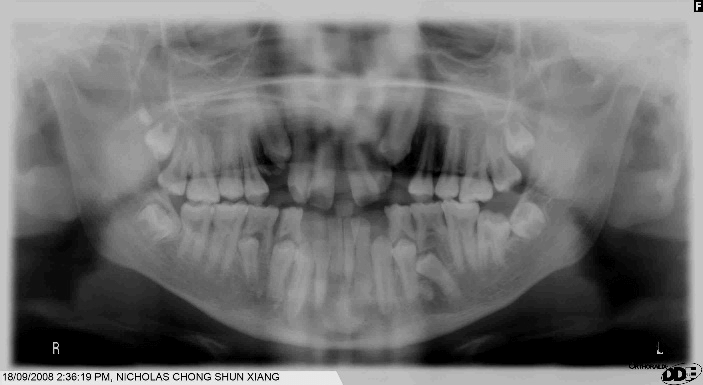
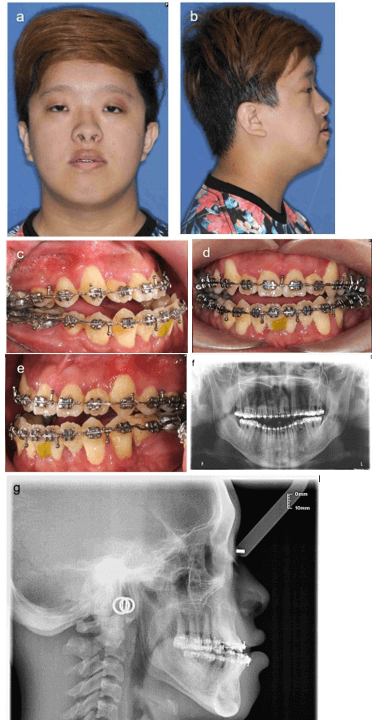
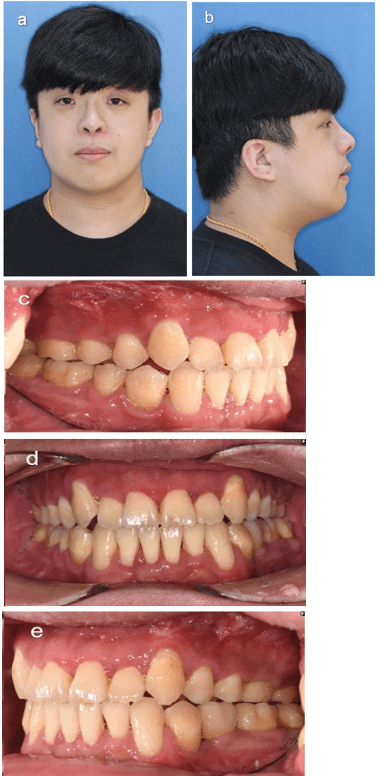
By age 17, the patient still had 9 unerupted permanent teeth including a dilacerated #35 (Figure 1). Orthodontic treatment commenced for space consolidation and he subsequently underwent multiple surgeries for removal of dilacerated #35 and all his impacted third molars; exposure and gold chain bonding of unerupted permanent teeth for orthodontic traction. The patient was subsequently planned for orthognathic surgery to correct his malocclusion and facial deformity. Following pre-surgical orthodontic preparation, he had a class III malocclusion with an overjet of -6mm and an anterior open bite (AOB) of 2.5mm. Skeletal analysis revealed a Skeletal III base with maxilla hypoplasia and mandible hyperplasia. He also presented with a low nasal dorsum, upturned tip, wide alar base and deviated nasal septum (Figure 2).
Figure 1: Orthopantomogram of patient at age 17 showing multiple unerupted permanent teeth.
Figure 2: A) Frontal view, B) right profile view, C) right buccal segment, D) anterior segment, E) left buccal segment, F) orthopantomogram, G) lateral cephalogram.
At age 23, he underwent orthognathic surgery: Le Fort 1 advancement of the maxilla of 5mm, anterior impaction of 1.5mm and posterior impaction of 3mm; bilateral sagittal split setback of the mandible with clockwise rotation of the maxilla-mandibular complex to close the AOB. 10 months after the orthognathic surgery, open septorhinoplasty was performed to correct the nasal deformities. Septal cartilage was harvested and used as an extended septal graft and columellar strut. Silicone implant was used to augment the dorsum height. Conchal cartilage from the left ear was harvested and used as only grafts for tip augmentation. Wedge excision of the ala base was performed to reduce the alar base width.
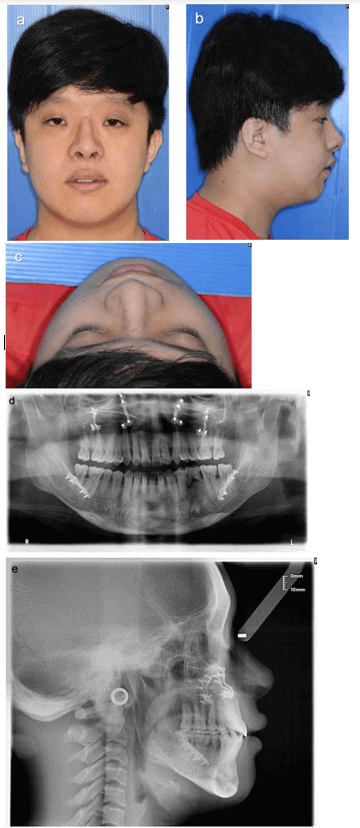
Figure 3: A) Frontal view, B) right profile view, C) bird’s eye view, D) orthopantomogram, E) lateral cephalogram.
Orthodontic treatment was completed 11 months after the orthognathic surgery. By then, the retained #75 which was mobile. It was extracted and planned for replacement with an implant-supported crown (Figure 3).
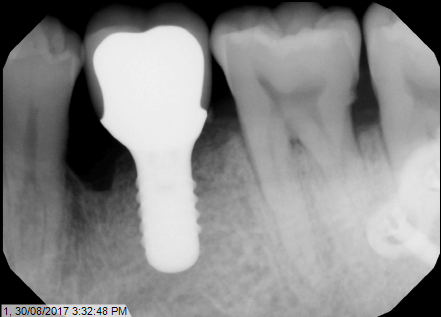
Figure 4: Dental implant at #35 region.
6 months after the open septorhinoplasty, revision rhinoplasty was done to correct the still slightly deviated nasal tip and hanging columella, and further reduce the alar base width. At the same surgery, a tissue level dental implant was inserted at #35 region and subsequently restored with an implant-supported crown (Figure 4).
Figure 5: A) Frontal view, B) right profile view, C) right buccal segment, D) anterior segment, E) left buccal segment.
His treatment was completed when he was 25 years of age. A 2-year follow-up showed that occlusion was stable, and patient was satisfied with the functional and aesthetic results (Figure 5).
Discussion
Management of dentofacial deformities of patients with CCD is a complex and long process, requiring a multi-disciplinary approach. Patients with CCD need regular dental reviews from a young age to monitor eruption of their permanent dentition as well as detection of supernumerary teeth that may obstruct the eruption of permanent teeth. These patients are usually followed-up by the orthodontist throughout their childhood and adolescence. When required, the oral and maxillofacial surgeon will be called to co-manage the buried teeth and subsequently, the orthognathic surgery. It is crucial to keep the patient motivated for their treatments and ensure they have a healthy expectation of the outcomes.
As patients with CCD often present with multiple buried supernumerary teeth and unerupted permanent teeth, there needs to be good communication between the orthodontist and oral and maxillofacial surgeon on which teeth to remove, keep or apply gold-chain bonding for tracking out. Use of 3D imaging to aid correct identification of teeth would be helpful. Even then, there is a risk of removing the wrong tooth or leaving behind teeth which have been indicated for removal. Hence, it would be prudent to inform the patient and/or parent of such risks during consent-taking. When in doubt, an intraoperative radiograph may be taken to confirm tooth identity, if dental radiologic equipment is available in the operating room.
Many CCD patients also suffer from maxillary hypoplasia and mandibular hyperplasia, giving them a Skeletal III facial deformity and Class III malocclusion. The treatment for these often requires combined orthodontics and orthognathic surgery. One intraoperative observation for this patient was that the maxillary sinus floor was noticeably more superiorly positioned than usual. Hence, when making the Le Fort I cut using the sagittal saw, thick “solid” bone was encountered, rather than the usual thin lateral wall of the maxillary sinus. Due to the “solid” maxilla, it was more difficult to down-fracture. This phenomenon was likely due to the patient having multiple buried teeth in the maxilla previously. This resulted in a vertically longer maxillary alveolus and a superiorly positioned sinus floor. Otherwise, there were no unusual problems encountered during the surgery.
Both staged and simultaneous rhinoplasty with orthognathic surgery have been described in the literature. The advantages of a simultaneous approach include (1) one general anaesthetic, operation and hospital stay, and (2) maxilla down-fracture allows better access for septoplasty, harvesting of the nasal septum and inferior turbinoplasty [3, 4].The disadvantages include (1) difficulty in predicting changes in the nasal position and morphology after maxillary repositioning, (2) difficulty in assessing nasal changes intraoperatively due to oedema, and (3) patient cannot be placed on inter-maxillary fixation post-operatively until after the nasal packs are removed, for airway safety [5].
For this patient, the rhinoplasty was done as a staged procedure. Orthognathic surgery may create or worsen an existing nasal abnormality. The patient underwent a Le Fort 1 maxillary advancement of 5mm and impaction. Maxillary advancement can result in raising the tip with an increase in the supratip break depression, widening the alar base, and worsening of the hanging columella. Maxillary impaction can result in raising the nasal tip and upper lip and widening the alar base [3, 6]. The large maxillary advancement in this case would make it difficult to predict the nasal and paranasal changes post-operatively. Sun and Steinbacher et al. recommended that staged rhinoplasty be performed in cases where there is maxillary advancement of more than 4 to 5mm [7].
Conclusion
The staged treatments for this patient resulted in a much-improved occlusion and facial aesthetics. The management of patients with CCD is challenging and long drawn. Successful treatment requires coordination of a multi-disciplinary team.
Article Info
Article Type
Case ReportPublication history
Received: Tue 12, May 2020Accepted: Mon 25, May 2020
Published: Thu 04, Jun 2020
Copyright
© 2023 Bee Tin Goh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.01
Author Info
Bee Tin Goh Mei Hui Tan Tian Ee Seah
Corresponding Author
Bee Tin GohDepartment of Oral & Maxillofacial Surgery, National Dental Centre Singapore, Singapore
Figures & Tables
References
- Ishii K, Nielsen IL, Vargervik K (1998) Characteristics of Jaw Growth in Cleidocranial Dysplasia. Cleft Palate Craniofac J 35: 161-166. [Crossref]
- Becker A, Lustman J, Shteyer A (1997) Cleidocranial Dysplasia: Part 1--General Principles of the Orthodontic and Surgical Treatment Modality. Am J Orthod Dentofac Orthop 111: 28-33. [Crossref]
- Cottrell DA, Wolford LM (1993) Factors Influencing Combined Orthognathic and Rhinoplastic Surgery. Int J Adult Orthodon Orthognath Surg 8: 265-276. [Crossref]
- Waite PD, Matukas VJ, Sarver DM (1988) Simultaneous Rhinoplasty Procedures in Orthognathic Surgery. Int J Oral Maxillofac Surg 17: 298-302. [Crossref]
- Seah TE, Bellis H, Ilankovan V (2012) Orthognathic Patients With Nasal Deformities: Case for Simultaneous Orthognathic Surgery and Rhinoplasty. Br J Oral Maxillofac Surg 50: 55-59. [Crossref]
- Mitchell C, Oeltjen J, Panthaki Z, Thaller SR (2007) Nasolabial Aesthetics. J Craniofac Surg 18: 756-765. [Crossref]
- Sun AH, Steinbacher DM (2018) Orthognathic Surgery and Rhinoplasty: Simultaneous or Staged? Plast Reconstr Surg 141: 322-329. [Crossref]
