Small Bowel Mesenteric Pseudocysts: Report of a Case and Review of the Literature
Small Bowel Mesenteric Pseudocysts: Report of a Case and Review of the Literature
A B S T R A C T
Background: Mesenteric pseudocyst (MP) are rare clinical entity presenting a thick fibrotic wall with internal septae without epithelial lining cells.
Case Report: We described one case of MP of a 50-year-old woman with persistent, non-specific, and non-responding to medical therapy abdominal pain. Laboratory tests, clinical examination and the abdominal US were un-conclusive while the CT scan of the abdomen showed a cystic lesion of the jejunal mesentery. We performed a laparoscopic surgical excision of the lesion with the resolution of clinical symptoms. The lesion resulted in inflammatory mesenteric cyst at the histological examination. At 5 years CT scan follow up we did not record any recurrences.
Conclusion: MP present themselves without specific symptoms, diagnostic imaging techniques such as US or CT scan may define its features, location or size but fail in determining their benign or malign nature. In fact, even if, the majority of these lesions are benign, a rate of malign transformation of around 3% has been reported, which is why the complete surgical excision is the gold standard treatment.
Keywords
Mesenteric pseudocyst, surgery, laparoscopy, abdominal pain
Introduction
The term “mesenteric cyst” refers to a heterogenous group of cystic lesions with different etiopathogenetic roots, which appears in the abdominal cavity or in the retroperitoneum without knowledge of its abdominal organ of origin. The mesenteric cyst is a rare entity, and its reported incidence ranges from 1 per 100.000 to 1 per 250.000 hospital admission [1]. Various classifications for this kind of lesions have been proposed. The term “mesenteric pseudocyst” (MP) was used for the first time by Ros et al. in their classification of mesenteric cysts; in 2000 de Perrot et al. introduced a classification based on the histological features of the internal epithelium and consisted of 6 groups: lymphatic cyst, mesothelial cyst, enteric cyst, urogenital cyst, mature cyst teratoma and pseudocyst [2, 3]. MP might have an infectious, traumatic, or even degenerative aetiology and is similar to pancreatic pseudocyst, from a histological point of view, presenting a thick fibrotic wall with internal septae without epithelial lining cells [3]. They are sited more frequently in the mesentery of the small bowel (50-80% of cases), colon (15-30%) or in the retroperitoneum (7-20%) [4].
Iida et al. reported in 2003 that the total number of MP’s records in Japanese literature was only 15 cases [5]. Yamabuki et al. reported in 2017 that the total number of MP records in the literature was about 20 cases [6]. In our report, we present the case of a woman with a jejunal MP and abdominal pain, who underwent a laparoscopic surgical procedure to excise the lesion and a concomitant review of the relevant literature.
Case Report
A 50-year-old female patient presented to our observation for the appearance of an abdominal cystic neoformation. The patients described diffuse abdominal pain for about 2 months without the association with any other gastrointestinal or general symptoms. The US of the abdomen was unfortunately vitiated by the subcutaneous fat and intestinal meteorism. An injected CT scan of the abdomen was carried out showing a cystic lesion (Figure 1) with a thick wall located in the mesentery of the small bowel in the right upper abdominal quadrant, which did not take contrast and appeared dissociable from the surrounding structures. His past medical history was remarkable for essential hypertension, while his surgical one was unremarkable. He had a BMI of 30 kg/m2 so the physical examination showed only a non-localized abdominal tenderness without signs of peritonitis; the laboratory tests were negative.
Figure 1: Abdominal CT scan frame showing cystic lesion with a thick wall located in the mesentery of the small bowel in the right upper abdominal quadrant, which did not take contrast and appeared dissociable from the surrounding structures.
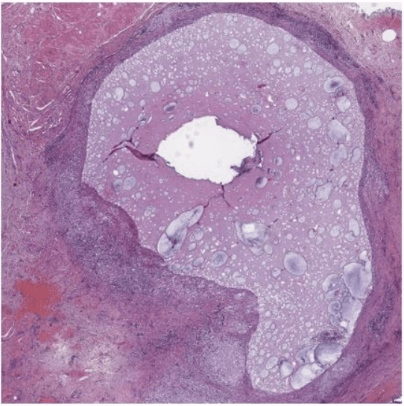
We performed a complete laparoscopic surgical excision of the lesion, which was located in the jejunal mesentery 30 cm distant from the Treitz ligament. The histological examination pleads in favour of the MP (Figure 2). The post-operatory course was uneventful, the patient was discharged on postoperative day 2 and the 5 years CT scan follow up did not show any recurrence. Moreover, at 6 months, clinical follow up the symptoms disappeared.
Figure 2: Hematoxylin-eosin, wholemount. Pseudocyst: cystic neoformation without epithelial or endothelial lining, with amorphous content showing fibrous and mucinous features and fibrotic wall, where a granulomatous inflammatory process can be detected (lymphocytes, histocytes, plasma cells, neutrophils).
Discussion
MPs are a rare entity, which usually occurs in the 4th decade in both sexes with equal frequency [7, 8]. Their size may vary from few to 30 centimetres; their pathogenesis remains unclear [9, 10]. Most authors support the hypothesis of a traumatic or infectious intestinal origin, in our case, both patients did not report any history of abdominal trauma or inflammatory disease. MPs are often asymptomatic and could be incidentally discovered during surgical procedure or ultrasound (US) and CT scan carried out for other reasons [6, 11].
At the physical examination, according to the patient’s habitus, we might not find any alteration, while sometimes, the lesion could disappear and reappear afterwards in a different location within the abdomen [12]. MP present non- specific symptoms such as abdominal pain (55-82%), abdominal lumps (44-61%) or might cause complications such as bleedings, volvulus or infections requiring an emergency surgical approach [4, 8, 9, 13-17].
US may be useful in the initial evaluation of the lesions providing information on its size and with high sensitivity on the presence of septation or debris inside it; nevertheless, it might fail the diagnosis it the MP is covered by intestinal loops. As a matter of fact, the T scan is more sensitive in terms of size, site and relation with neighbouring organ definition. Ayyappan et al. showed the utility of chemical shift MRI in detecting the lipid content of MP [18]. All MPs are benign lesions, except for the malign cystic mesothelioma, an extremely rare entity [3]. However, an incidence rate of malignant mesenteric cyst of approximately 3% has been reported; therefore, given the impossibility of excluding the malignant nature with the imaging technique or laboratory tests, it is advisable to surgically excise even the smaller MP [3, 19, 20]. The complete surgical excision of MPs, both with a laparoscopic and open surgical approach, is associated with partial resection of the bowel in the event they are non-dissociable; it is the treatment of choice. The laparoscopic approach should be preferred and the conversation to an open one is rare. Chandradevon et al. recently reported a case of MP successfully treated with the robotic approach [6, 21]. From a review of the cases reported in the literature, after complete excision of the MPs recurrences have not been observed.
Conclusion
MPs are an extremely rare entity; given the lack of pathognomonic clinical, laboratory and imaging features, surgical excision is advisable due to the risk of complications and malignant transformation and a laparoscopic approach should be preferred.
Author Contributions
All authors contributed to the study; Geraci G. and Di Vita G. conceived, devised and designed the manuscript; D’Orazio B., Bonventre S. and Cudia B. collected the case and iconography; D’Orazio B. and Geraci G. wrote the manuscript and participated in the sequence alignment; Di Vita G., Sciumé C. and Martorana G. revised and approved the final manuscript and its conclusions.
Disclosure
This article has not been presented nor published elsewhere.
Funding
None.
Competing Interests
None.
Conflicts of Interest
None.
Consent
An informed written consent was obtained from all individual participants included in this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 24, Aug 2020Accepted: Wed 09, Sep 2020
Published: Mon 21, Sep 2020
Copyright
© 2023 Gaetano Di Vita. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.09.13
Author Info
Beatrice D'Orazio Bonventre Sebastiano Martorana Guido Cudia Bianca Sciumé Carmelo Gaetano Di Vita Geraci Girolamo
Corresponding Author
Gaetano Di VitaGeneral Surgery Unit, Department of Surgical, Oncological and Stomatological Sciences, University of Palermo, Italy
Figures & Tables

References
- V W Vanek, A K Phillips (1984) Retroperitoneal, mesenteric, and omental cysts. Arch Surg 119: 838-842. [Crossref]
- P R Ros, W W Olmsted, R P Moser Jr, A H Dachman, B H Hjermstad et al. (1987) Mesenteric and omental cysts: histologic classification with imaging correlation. Radiology 164: 327-332. [Crossref]
- M de Perrot, M Bründler, M Tötsch, G Mentha, P Morel (2000) Mesenteric cysts. Toward less confusion? Dig Surg 17: 323-328. [Crossref]
- M S Saviano, S Fundarò, R Gelmini, G Begossi, S Perrone et al. (1999) Mesenteric cystic neoformations: report of two cases. Surg Today 29: 174-177. [Crossref]
- Toshio Iida, Masahiro Suenaga, Yuki Takeuchi, Toru Kobayashi, Jyunichi Tobinaga et al. (2003) Mesenteric pseudocyst of the sigmoid colon. J Gastroenterol 38: 1081-1085. [Crossref]
- Takumi Yamabuki, Masato Suzuoki, Tsuzuku Murakami, Satoshi Hirano (2017) Laparoscopic Resection of a Jejunal Mesenteric Pseudocyst. Case Rep Gastroenterol 11: 526-530. [Crossref]
- G Resta, D Tartarini, N Fabbri, E Bianchini, G Anania (2014) Laparoscopic resection of a jejunal mesenteric pseudocyst: case report. G Chir 35: 279-282. [Crossref]
- R J Kurtz, T M Heimann, J Holt, A R Beck (1986) Mesenteric and retroperitoneal cysts. Ann Surg 203: 109-112. [Crossref]
- Jacqueline Oxenberg (2016) Giant Intraperitoneal Multiloculated Pseudocyst in a Male. Case Rep Surg 2016: 4974509. [Crossref]
- Jane Jye Yng Tan, Ker Kan Tan, Soo Ping Chew (2009) Mesenteric cysts: an institution experience over 14 years and review of literature. World J Surg 33: 1961-1965. [Crossref]
- Sang Eok Lee, In Seok Choi, Won Jun Choi, Dae Sung Yoon, Ju Ik Moon et al. (2012) Mesenteric pseudocyst of the small bowel in gastric cancer patient: a case report. J Gastric Cancer 12: 43-5. [Crossref]
- Jasneet Singh Bhullar, Paraskevi Orfanou (2014) The disappearing abdominal mass: mesenteric pseudocyst. JSLS 18: 319-322. [Crossref]
- H L Fan, T W Chen, Z J Hong, C B Hsieh, D C Chan et al. (2009) Z Volvulus of small intestine: rare complication of mesenteric pseudocyst. Z Gastroenterol 47: 1208-1210. [Crossref]
- S Boopathy Vijayaraghavan, Valkodai Ramanathan Ravikumar, Gopalakrishnan Srimathy (2004) Whirlpool sign in small-bowel volvulus due to a mesenteric cyst. J Ultrasound Med 23: 1375-1377. [Crossref]
- Wen I Liao, Yen Yue Lin, Kai Hsiung Ko, Shi Jye Chu, Shih Hung Tsai (2009) Midgut volvulus as a delayed consequence of posttraumatic mesenteric pseudocyst. Am J Emerg Med 27: 1025.e3-1025.e6. [Crossref]
- Martín Adrián Bolívar Rodríguez, Marcel Antonio Cazarez Aguilar, Eduardo Esaú Luna Madrid, Fred Morgan Ortiz (2015) Infected jejunal mesenteric pseudocyst: A case report. Cir Cir 83: 334-338. [Crossref]
- Thomas Serena, Raisa Gao, Kelly Dinnan (2020) Open surgical approach for infected mesenteric pseudocyst presenting as lifelong, migratory abdominal pain-A case report. Int J Surg Case Rep 66: 96-100. [Crossref]
- Anoop P Ayyappan, Kartik S Jhaveri, Masoom A Haider (2011) Radiological assessment of mesenteric and retroperitoneal cysts in adults: is there a role for chemical shift MRI? Clin Imaging 35: 127-132. [Crossref]
- Jacek Kurnicki, Janusz Swiątkiewicz, Natalia Wrzesińska, Maciej Skórski (2011) Laparoscopic treatment of a huge mesenteric pseudocyst - case report. Wideochir Inne Tech Maloinwazyjne 6: 167-172. [Crossref]
- Seong Eun Park, Tae Joo Jeon, Ji Young Park (2014) Mesenteric pseudocyst of the transverse colon: unusual presentation of more common pathology. BMJ Case Rep 2014: bcr2013202682. [Crossref]
- Raguraj Chandradevan, Ian Rutkofsky, Kristal Sirju, Felisha L Kitchen, John T Williams (2019) Look Before You Leap": Robotic Resection of a Jejunal Mesenteric Pseudocyst. Cureus 11: e4750. [Crossref]
