Pilomatrixoma: A Case Study & Review of Literature
Pilomatrixoma: A Case Study & Review of Literature
A B S T R A C T
Pilomatrixoma, or calcific epithelioma of Malherbe, is a rare benign subcutaneous tumor of adnexal origin. Females are twice as affected as males. The authors carry out a review of the literature on the subject and present a clinical case. It is a 60-year-old patient with this type of tumor on the medial aspect of her left leg, who was operated on an outpatient basis two years ago and currently has no recurrence. Diagnosis is often difficult to make clinically, and therefore can only be definitively established after histopathological examination of the lesion after surgical removal. Ultrasound role is to validate the clinical diagnosis, exclude pathologies with similar clinical presentations, and establish the relationship of the lesion with the surrounding structures.
Keywords
Ghost cell, pilomatrixoma, skin neoplasm, ossification
Introduction
Also known as Malherbe's benign calcifying epithelioma, this is a rare benign tumor that arises from the hair root matrix. It was first described by Malherbe and Chenantais in 1880 [1]. Pilomatrixoma, or Malherbe calcific epithelioma, is a benign subcutaneous tumor of adnexal origin. It typically presents as a solitary, asymptomatic lump, most often located on the face and neck. A pilomatrixoma is a small, solid subcutaneous mass that shows up under the skin. It most commonly occurs as a single bump located on the face, scalp, eyelids, eyebrows, neck, or arms, but in some cases, it can be multiple.
It has variable dimensions between 0.5 and 3 cm, although cases of more than 10 cm have been reported in the literature and occasionally may show signs of inflammation. It generally affects young people (first and second decade) and is more frequent in women. Most cases of pilomatrixoma occur in children under the age of 10, but it can also be present in older children and young adults. Females are twice as likely as males to have pilomatrixoma. In addition to the solitary form, it can occur in multiple forms [1, 2].
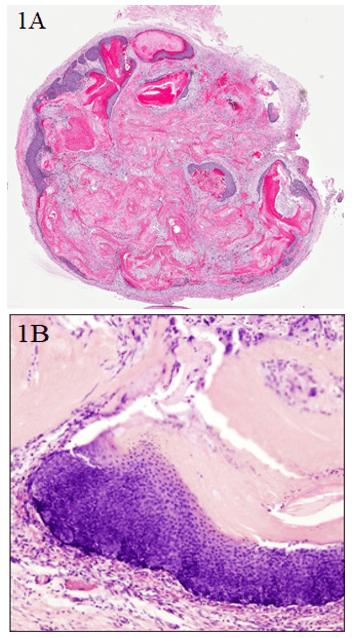
Histologically it appears well-demarcated, consisting of islets of epithelial cells immersed in stromal cells, located in the dermis or subcutaneous fat (Figure 1). Basophilic cells are present in the periphery while in the center, there are mummified cells called "ghost" cells or "shadow" cells, which filled with keratin, have lost their nucleus and often have calcium deposits. The transitional cells, located between basophil cells and shadow cells, appear to represent apoptotic cells that will eventually become shadow cells. The stroma appears instead to be made up of collagen and contains vessels [3]. It does not present aggressive characteristics and the treatment is surgical with resection margins of at least 1-2 cm to prevent a recurrence, which is frequent in the case of incomplete resection [4].
Although the diagnosis of certainty is made only with histological examination, ultrasound can help the clinical setting. Pilomatrixomas have been found familiar in some cases or seen in association with inherited genetic syndromes. There is no primary prevention.
Diagnosis
Diagnosis is often difficult to create clinically, and therefore can only be definitively established after histopathological examination of the lesion after surgical removal. It usually appears as a slowly widening mass under the skin, less than 3 cm in diameter. There is usually no associated pain, excessive skin inflammation, or change in skin colour. Less commonly, the lesion can become inflamed or infected and cause discomfort at that time. A few case reports have described injuries presenting as bruising after trauma, with some authors suggesting this may be a more aggressive variant of the injury. In contrast, a survey by Orlando et al. described 150 cases of pilomatrixoma in a children's hospital that had no history of trauma or inflammation [5, 6].
Physical Examination
A subcutaneous nodule often less than 3 cm in diameter under the skin in locations typical of the eyelids, eyebrows, scalp, glabella, or neck; other positions are seen less commonly. The nodule is round, smooth, very hard and freely movable on the underlying bone. The overlying skin may be thin and adherent to the anterior face of the lesion. It is not strained for palpation. The overlying skin is usually normal, with no dilated blood vessels, inflammation, or ulceration. Some reports have described a red-blue or bluish-purple skin discolouration to be more typical of pilomatrixoma, which could differentiate it from dermoid inclusion and cysts. Inclusion cysts tend to have a diffuse yellow colour due to the keratin within the cyst and are softer and fluctuating [7].
The skin on capillary hemangiomas in the subcutaneous tissue will often have a blue-purple hue that can sometimes be seen as pilomatrixoma, but a capillary hemangioma is softer than a pilomatrixoma. Rhabdomyosarcoma may rarely present as an eyelid mass, but typically has skin erythema and is an extension of deep orbital tissue involvement [8, 9].
Diagnostic Procedures
Pathological evaluation of the surgical specimen is necessary to make the definitive diagnosis, although clinical findings are usually typical of pilomatrixoma. On ultrasound examination, pilomatrixoma appears as a generally oval lesion, with well-defined margins, inhomogeneous due to the presence of anechoic areas of cystic degeneration and point-like hyperechoic images due to calcifications. It has a posterior shadow cone and a hypoechoic edge that corresponds to the connective capsule [1-3]. The differential diagnosis is with the epidermoid cyst, a hypoechoic mass devoid of vascularization demonstrable with Colour-Doppler, with hemangioma: which has a soft consistency, lobulated contours, and calcifications, if present, are rounded; with lymph node hyperplasia: which generally has hilar vascularity and is uniformly hypoechoic; with ossifying hematoma: markedly hyperechoic with posterior shadow cone and absence of vascularization; with dermatofibrosarcoma: generally devoid of calcifications [3, 4, 10].
Lab Test
Blood tests are not indicated. Images such as X-Ray, CT, or MRI are often not done as the clinical examination is often indicative of the injury before surgery.
Differential Diagnosis
It is carried out against:
i Dermoid cyst;
ii Epidermoid cyst;
iii Inclusion cyst;
iv Chalazion;
v Lipoma;
vi Fibroma;
vii Bone cyst;
viii Hematoma;
ix Capillary soft tissue hemangioma;
x Cholesterol granuloma;
xi Malignant tumor (rhabdomyosarcoma).
Histopathology
Histopathology demonstrates a pseudo-encapsulated mass with eosinophilic acellular material with prominent ghost ("shadow") cells. Granulomas and small foreign body giant cell calcifications may be present in the lesion. Nests of basaloid cells with small cytoplasm comprise the periphery of the lesion and form keratinous material (Figures 1A & 1B) [11, 12].
Figure 1: A) Microscopic appearance with basaloid cell nests. Basaloid areas showing focal area differentiation with compact red keratin (10 x input). B) Basaloid cells at higher magnification (40 x). Hematoxylin/Eosin staining.
Clinical Case Study
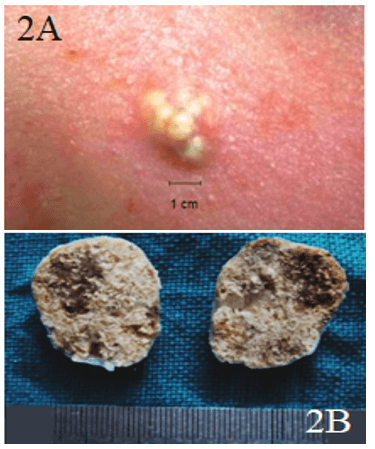
We described a clinical case to explain the feasibility and safety of the surgical procedure. In November 2018, we admitted a 60-year-old patient (AC) with a 2.5 × 2.5 cm lump in her left leg at the calf (Figures 2A & 2B). PMH: arterial hypertension; BMI: 33; ASA 2. The lesion had a hard and mobile consistency on the deep planes. The patient agreed to surgical removal. He also agreed to collect and register his data in an electronic database for proper analysis. The operation was performed under local anaesthesia.
Figure 2: A) Preoperative aspect; B) macroscopic aspect.
Therapy
Observation is reasonable unless the lesion enlarges and becomes symptomatic. A pilomatrixoma will not resolve spontaneously or with involution; therefore, surgical excision is the treatment of choice for symptomatic or progressively increasing lesions. No medical treatment can be adopted.
Surgery
Surgery is the treatment for the complete removal of the lesion. This is usually curative and also allows for pathological diagnosis of the mass. In the eyelid or eyebrow region, the lesion can often be removed via an incision in the crease of the eyelid. The procedure is often performed as outpatient day surgery, with the patient returning home after the surgery. The lesion is removed in its entirety and sent in 10% Formaldehyde for histopathological evaluation. Routine postoperative care generally requires rest, sterile compresses on the surgical site, and antibiotic ointment for the sutures. Pain is often minimal.
Figure 3: Postoperative aspect three months after surgery.
The prognosis after surgical removal is excellent (Figure 3), but in some cases, the reports have shown a very low recurrence rate. Patients and their families should be aware that any new lesions must be appropriately evaluated.
Conclusion
Pilomatrixoma is therefore a relatively rare lesion whose diagnosis is clinical and histological; the role of ultrasound is to validate the clinical diagnosis, exclude pathologies with similar clinical presentations, and establish the relationship of the lesion with the surrounding structures.
Acknowledgements
None.
Conflicts of Interest
None.
Consent
Consent to publication was taken from the patient.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Tue 25, Aug 2020Accepted: Wed 09, Sep 2020
Published: Tue 29, Sep 2020
Copyright
© 2023 Alessandro Crisci. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.09.14
Author Info
Alessandro Crisci Michela Crisci
Corresponding Author
Alessandro CrisciDepartment of Medicine, Surgery and Dentistry “Salernitan Medical School”, University of Salerno, Fisciano (SA), Italy
Figures & Tables

References
- Malherbe A, Chenantais J (1880) Note sur l'epitheliome calcife des glandes sebacees. Prog Med (Paris) 8: 826-837.
- Moehlenbeck F W (1973) Pilomatrixoma (calcifying epithelioma). A statistical study. Arch Dermatol 108: 532-534. [Crossref]
- Macleod A J, Scobie W G (1991) Pilomatrixoma as a diagnostic problem: the Edinburgh experience. J Roy Coll Surg Edinb 36: 261-263. [Crossref]
- Mathen L C, Olver J M, Cree I A (1999) A large rapidly growing pilomatrixoma on a lower eyelid. Br J Ophthalmol 84: 1203-1204. [Crossref]
- Orlando R G, Rogers G L, Bremer D L (1983) Pilomatixoma in a paediatric hospital. Arch Ophthalmol 101: 1209-1210. [Crossref]
- Inglefield C J, Muir I F, Gray E S (1994) Aggressive pilomatrixoma in childhood. Ann Plas Surg 33: 656-658. [Crossref]
- Rotenberg M, Laccourreye O, Cauchois R, Laccourreye L, Putterman M et al. (1996) Head and neck pilomatrixoma. Am J Otolaryngol 17: 133-135. [Crossref]
- Shields J A, Shields C L, Eagle R C Jr, Mulvey L (1995) Pilomatrixoma of the eyelid. J Pediatr Ophthalmol Strabismus 32: 260-261. [Crossref]
- Yap E Y, Hohberger G G, Bartley G B (1999) Pilomatrixoma of the eyelids and eyebrow in children and adolescents. Ophthalmic Plast Reconstr Surg 15: 185-189. [Crossref]
- Yoshimura Y, Obara S, Mikami T, Matsuda S (1998) Calcifying epithelioma (pilomatrixoma) of the head and neck: an analysis of 37 cases. Br J Oral Maxillofac Surg 35: 429-432. [Crossref]
- Zaman S, Majeed S, Rehman F (2009) Pilomatricoma-Study on 27 cases and review of literature. Biomedica 25: 69-72.
- Ghartimagar D, Ghosh A, Gautam K, Thapa S, Shrestha SR et al. (2014) Clinicopathological features of pilomatricoma cases: Analysis of 21 cases. J Pathol 4: 530-533.
