Journals
Inopportune Opportunism: First Diagnosis of AIDS in New-Onset Viral Myocarditis
A B S T R A C T
Opportunistic infections from cytomegalovirus (CMV) are a possible manifestation of late-stage AIDS. We present a case of acute CMV myocarditis, which eventually allowed for the diagnosis of a previously unknown HIV infection.
Keywords
Myocarditis,viral,HIV,AIDS,CMV,opportunistic,endomyocardial biopsy,cardiac magnetic resonance,arrhythmias
Introduction
Opportunistic infections from cytomegalovirus (CMV) are a possible manifestation of late-stage AIDS, when CD4+ blood count falls below 50-100/mm3 [1]. We present a case of acute CMV myocarditis, which eventually allowed for the diagnosis of a previously unknown HIV infection.
Case Presentation
A 59-year old male with hypertension and type-2 diabetes mellitus presented to emergency room (ER) with acute heart failure. His past medical history was remarkable for ischaemic heart disease: eight years ago, after incidental finding of left bundle branch block (LBBB) at screening ECG, echocardiogram showed left ventricular systolic dysfuncion (LVEF 40%) with stress/rest myocardial scintigraphy positivity for inducible ischaemia. Coronary angiography was performed, showing critical stenosis at proximal left anterior descending artery and mid right coronary artery, treated by transcatheter angioplasty and double drug eluting stent implant. Furthermore, five years ago the patient was also diagnosed with dysmetabolic fatty liver disease (negative screening for HIV/HBV/HCV).
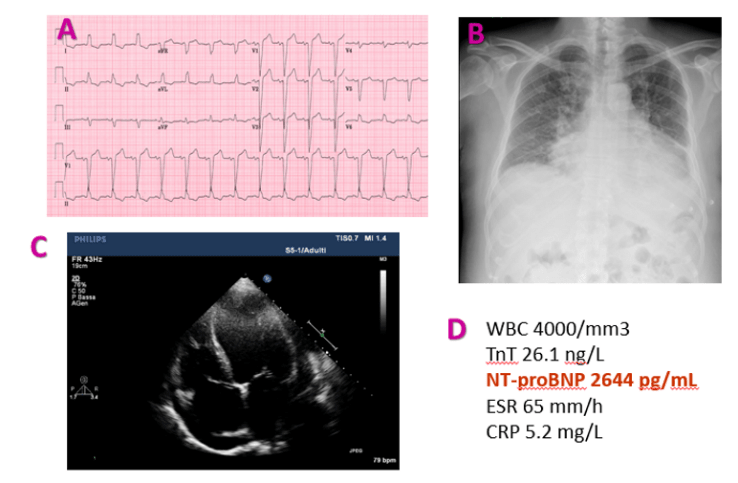
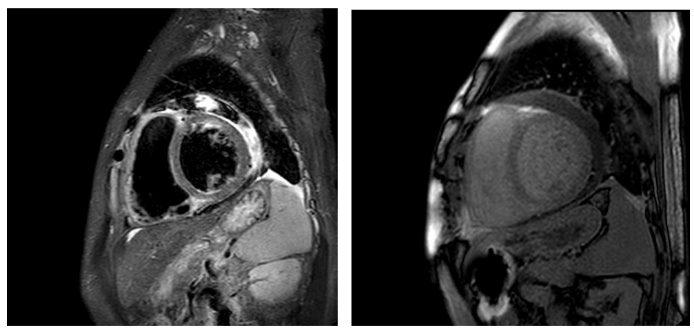
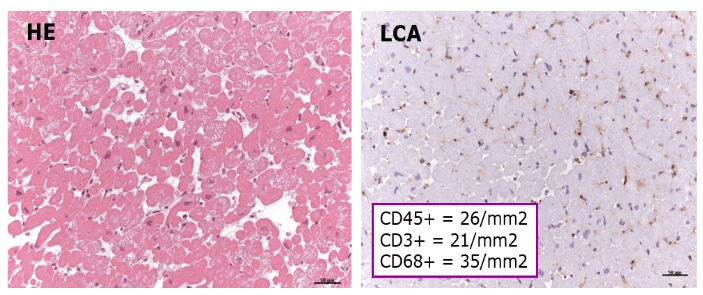
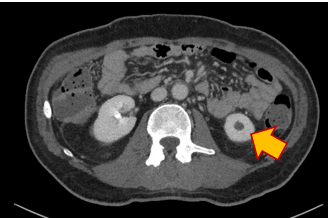
At current ER access, the patients was symptomatic for acute dyspnoea, ankle swelling and weight gain. At presentation, ECG showed normal sinus rhythm with known LBBB (Figure 1A). Chest X-ray was significant for cardiomegaly and signs of pulmonary oedema (Figure 1B). Transthoracic echocardiogram showed severe LV dilation and systolic dysfunction (LVEDV 240 mL; LVEF 15%) with no regional wall motion abnormalities (Figure 1C). Blood exams results are shown in (Figure 1D). Since T troponin (TnT) was near-normal (url < 14 ng/L), the patient did not undergo coronary angiography. Instead, CMR was performed, showing both myocardial oedema at T2/STIR sequences and nonischaemic late gadolinium enhancement, in particular at mid-basal segments of anteroseptal LV wall extending to the right ventricle, suggesting a diagnosis of active myocarditis (Figure 2) according to the Lake Louise criteria [2]. Endomyocardial biopsy (EMB) was then performed, showing acute lymphocytic myocarditis according to the European Society of Cardiology (ESC) criteria [3]. Molecular biology analysis showing positivity for CMV genome. Since CMV myocarditis is quite uncommon in the immunocompetent host, intense diagnostic workup was performed, allowing for identification of a severe CD4+ T-cells leukopenia (87/mL; total WBC 4,000/mL) together with high-load replicating CMV copies in blood. AIDS was subsequently suspected: ELISA and Western blot tests eventually confirmed a previously unknown HIV infection. Further CMV organ localizations (liver, eye, brain, adrenal glands) were accurately excluded (Figure 4). The patient was treated by iv valgancyclovir together with HAART. After 3 weeks, complete CMV blood clearance, LV reverse remodeling (170 mL; LVEF 30%) and significant NT-proBNP reduction (from 2644 to 460 pg/mL) were observed.
Figure 1: ECG (A), chest XR (B), TT echocardiogram (C) and lab exams (D) at presentation.
Figure 2: CMR (T2/STIR; LGE) shows active myocarditis.
Figure 3: EMB shows myocarditis (haematoxylin/eosin; IHC for leucocyte common antigen).
Figure 4: Imaging screening for CMV end-organ localization. Note incidental finding of left adrenal mass (arrow).
Discussion
Two critical features made this clinical case particularly difficult: a) because of known ischaemic heart disease and multiple CV risk factors, pre-test probability of myocarditis was relatively low; b) 5 years ago a negative HIV test was obtained. However, in the presence of acute heart failure with mild troponin alteration and no regional wall motion alterations, CMR was the exam of choice instead of coronary angiography and showed signs of inflammatory heart disease. However, EMB only allowed for an aetiology-driven treatment. In the end, it was possible to diagnose a complex systemic disease, such as AIDS, thanks to a complex diagnostic workup entirely held in Coronary Care Unit.
Conclusion
When active myocarditis is suspected, EMB is still the gold standard for aetiologic diagnosis and subsequent targeted treatment. In the presence of unexplained CMV+ myocarditis, especially together with an even mild leukopenia, HIV test is strongly recommended for the best diagnostic and therapeutic workup of the patient.
Funding
This case report was not funded.
Disclosures
The authors declare that there is no conflict of interest.
Article Info
Article Type
Case ReportPublication history
Received: Sat 29, Jun 2019Accepted: Wed 31, Jul 2019
Published: Mon 12, Aug 2019
Copyright
© 2023 Giovanni Peretto. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2019.03.04
Author Info
Giovanni Peretto Massimo Slavich
Corresponding Author
Giovanni PerettoDepartment of Cardiac Electrophysiology and Arrhythmology, IRCCS San Raffaele Hospital and University, Milan, Italy
Figures & Tables


References
- Saag MS, Masur H (2014) HIV/AIDS. Infect Dis Clin North Am 28: ix-x. [Crossref]
- Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P et al. (2009) Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol 53: 1475-1487. [Crossref]
- Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J et al. (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 34: 2636-2648. [Crossref]
