Head and Neck MRI Imaging Performed Safely in a Patient with Sacral Neuromodulation Device: A Case Report
A B S T R A C T
Introduction: Sacral neuromodulation is a well-established treatment option to manage refractory lower urinary tract and pelvic floor disorders. The technique involves implantation of a lead and an internal pulse generator that delivers electrical impulses to modulate the sacral area. Many patients worldwide have been implanted with MRI-non-compatible devices. Currently, MRI head only can be performed safely in these patients. Therefore, we present a case report of a patient who underwent MRI of the head as well as neck in the presence of a sacral neuromodulator without serious complications.
Case Report: A 33-year-old lady known to have systemic lupus erythematosus, refractory overactive bladder, and recurrent urinary tract infection started complaining of right sided neck pain for 3 months in which she required MRI of the head and neck to further assess the nature of the pain. The patient was already implanted with sacral neuromodulator with excellent outcome to manage her refractory overactive bladder. Following careful discussion with the patient and radiologist, MRI study was conducted at 1.5 tesla and total procedure duration was 8 minutes for T1, T2 sagittal and axial cuts. The patient revealed feeling minimal tingling of the right lower limb and mild lower back pain during MRI, all of which disappeared once the study was terminated. Device was functioning well afterwards.
Conclusion: MRI may be feasible for certain sacral neuromodulation patients under certain conditions without any serious adverse events.
Keywords
Sacral neuromodulation, MRI, device safety
Introduction
Sacral neuromodulation is a well-established modality for managing refractory lower urinary tract and pelvic floor disorders. It works by permanently implanting a lead and an internal pulse generator which delivers electrical impulses to modulate the sacral area. Although MRI-compatible devices are emerging recently, most of the patients worldwide have been implanted with MRI-non-compatible devices. The manufacturer demonstrated that MRI examinations of the head only may be safely performed under certain conditions. Thus, we present a case who underwent MRI of the head as well as neck in the presence of a sacral neuromodulator without serious complications.
Case Report
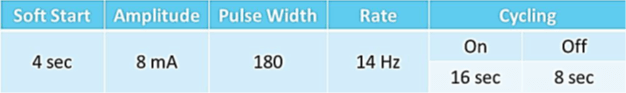
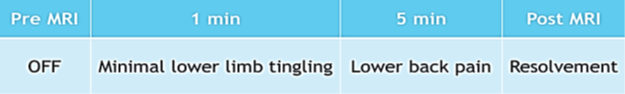
A 33-year-old lady known to have systemic lupus erythematosus, refractory overactive bladder, and recurrent urinary tract infection started complaining of right sided neck pain for 3 months. Full history, examination, and laboratory investigations were conducted. In addition, ultrasound of the neck was done. She was referred for magnetic resonance imaging (MRI) of the head and neck if no contraindications. The patient had sacral neuromodulation (SNM) device implantation two years ago for her refractory bladder over-activity symptoms excellent outcome. She was mainly using a device programme setting of amplitude of 8mA, power 180, and rate of 14Hz (Table 1). Following careful discussion with the patient and radiologist we decided to proceed with MRI to include the head and neck. Risks and benefits were explained to the patient and written consent was obtained. MRI study was conducted at 1.5 tesla and total procedure duration was 8 minutes for T1, T2 sagittal and axial cuts. During the procedure, the SNM device was switched off. One minute after commencing MRI, the patient was feeling minimal tingling of the right lower limb, and after three minutes she started complaining of minimal lower back pain described as 3 out of 10 on pain scale. Following the MRI study, the implanted device was switched on and patient reported full functioning of the device with same pre-study programme parameters and complete disappearance of the tingling and pain symptoms (Table 2).
Table 1: Sacral neuromodulation device programme pre and post MRI.
Table 2: Patient reported symptoms during MRI study.
Discussion
SNM with InterStim (Medtronic, Minneapolis, Minnesota, USA) is a Food and Drug Administration (FDA) approved and well established third line therapy for patients with chronic voiding dysfunctions in the form of urinary urge incontinence, urgency frequency syndrome and non-obstructive urinary retention. MRI has been evolving as the diagnostic procedure of choice for evaluating patients with suspected disease involving the central nervous system, spinal cord, and soft tissue evaluation. Moreover, magnetic resonance angiography also is becoming a commonly used tool for evaluating the cerebrovascular circulation. However, undergoing MRI for patients with an implantable device is challenging, especially when imaging is needed adjacent to the device location. The manufacturer of InterStim demonstrated that MRI examinations of the head only may be safely performed under certain conditions [1]. Exposing a patient with an implanted device, MRI could potentially cause pain or discomfort to the patient or damage to the nerve fibers at the site of the implanted electrodes.
Several studies conducted on pacemakers, implantable cardioverter defibrillators, cochlear implants, spinal cord stimulators, deep brain stimulators, vagus nerve stimulators, and pelvic neurostimulators have not shown major malfunctions, while others reported some malfunctions following MRI examinations [2-5]. Some studies have reported that during MRI session, no patient showed symptoms requiring stopping the examination and there was no change in perception of the stimulation after reprogramming of the implanted sacral nerve stimulator, according to patients’ feedback. Devices were functioning properly, and no change in bladder function was reported afterwards. No significant adverse events were encountered in patients implanted with SNM who underwent a 1.5 tesla lumbosacral MRI scan. Therapeutic efficacy of sacral neuromodulation was unchanged 1 month after imaging [6, 7].
Conclusion
In our case, we managed to avoid removing a perfectly functional SNM device. The case showed that MRI could be safely extended beyond the head to include the neck area in a patient with SNM device. Although MRI-compatible SNM devices are emerging recently, most of SNM patients worldwide so far are implanted with the old MRI-non-compatible (unsafe) devices making this a valid point. Our report suggests that MRI may be feasible for certain SNM patients under certain conditions without any serious adverse events.
Article Info
Article Type
Case ReportPublication history
Received: Mon 31, May 2021Accepted: Fri 25, Jun 2021
Published: Fri 23, Jul 2021
Copyright
© 2023 Tariq F. Al-Shaiji. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.07.05
Author Info
Hussain Al-Rashed Tariq F. Al-Shaiji
Corresponding Author
Tariq F. Al-ShaijiUrology Unit, Department of Surgery, Amiri Hospital, Kuwait City, Kuwait
Figures & Tables
References
1.
Medtronic (2012)
MRI Guidelines for InterStim Therapy neurostimulation systems.
2.
Luechinger R,
Duru F, Scheidegger MB, Boesiger P, Candinas R (2001) Force and torque effects
of a 1.5-Tesla MRI scanner on cardiac pacemakers and ICDs. Pacing Clin Electrophysiol 24: 199-205. [Crossref]
3.
Muehling OM,
Wakili R, Greif M, von Ziegler F, Morhard D et al. (2014) Immediate and 12
months follow up of function and lead integrity after cranial MRI in 356
patients with conventional cardiac pacemakers. J Cardiovasc Magn Reson 16: 39. [Crossref]
4.
Rezai AR, Finelli
D, Nyenhuis JA, Hrdlicka G, Tkach J et al. (2002) Neurostimulation systems for
deep brain stimulation: in vitro evaluation of magnetic resonance
imaging-related heating at 1.5 tesla. J
Magn Reson Imaging 15: 241-250. [Crossref]
5.
Thornton JS
(2017) Technical challenges and safety of magnetic resonance imaging with in
situ neuromodulation from spine to brain. Eur
J Paediatr Neurol 21: 232-241. [Crossref]
6. Elkelini MS, Hassouna MM (2006) Safety of MRI at 1.5Tesla in patients with implanted sacral nerve neurostimulator. Eur Urol 50: 311-316. [Crossref]
7. Guzman Negron JM, Pizarro Berdichevsky J, Gill BC, Goldman HB (2018) Can Lumbosacral Magnetic Resonance Imaging be Performed Safely in Patients with a Sacral Neuromodulation Device? An In Vivo Prospective Study. J Urol 200: 1088-1092. [Crossref]
