Capacity Building for the Diagnosis and Management of Cardiac Arrhythmias in Africa
A B S T R A C T
Cardiac Arrhythmias (CA) are major cause of death and disability worldwide. In Africa, a continent of poor resources, there is lack of trained specialists for adequate management of these patients. In this article, we propose a practical approach for capacity building of general practitioners to improve easy and timely recognition and better management of CA in Africa.
Keywords
Capacity building, general practitioners, diagnosis, management, cardiac arrhythmias
Introduction
Cardiac Arrhythmias (CA) are major cause of death and disability worldwide [1]. Atrial fibrillation, bradyarrhythmias, and conduction system diseases account for the most rhythm conditions [2]. In Africa, the rate of CA increased gradually following the epidemiological transition of diseases [3]. According to a recent systematic review conducted by Matthew F. Yuyun et al., there are few available health professionals who can adequately manage CA in Africa [4]. In fact, the cardiopulmonary resuscitation awareness for the management of cardiac arrest is generally low and there is scarcity of cardiac implantable electronic devices insertions and invasive arrhythmia treatment centers [4]. Bonny et al. in 2019 identified the low number of trained clinicians who could detect and manage CA [5]. Given the lack of task forces for CA management in Africa; it is important to propose a practical approach to build the capacity of all general practitioners for adequate recognition of CA and manage it early [6].
Challenges in the Management of Cardiac Arrhythmia in Africa
There is scarcity of data about the general gap in the management of Cardiac Arrhythmia in Africa. The World Heart Federation (WHF) identifies three main areas of care gaps in the management of Atrial Fibrillation (AF) in low- and middle-income countries (LMICs) including inadequate screening for AF among high-risk individuals, low rates of treatment initiation of anticoagulation, and the lack of country specific AF data to tailor interventions [7]. Concerning Bradyarrhythmia, the two main problems reported by Mkoko et al., is the lack of trained specialists for cardiac stimulation and the high cost of the procedure [3]. The challenge of prevention of sudden cardiac death in Africa mainly concerns incorrect consideration of antiarrhythmic drugs as equally to intracardiac defibrillator and the high cost of this procedure. With important efforts made by some African cardiac societies, the field of cardiac arrhythmia will probably interest more practitioners in the future [6]. As cardiovascular diseases increase significantly in Africa; it is urgent to propose a cost-effective and context-specific practical approach geared at the better diagnosis and management of cardiac arrhythmia using the limited resources available in Africa [8].
Building Capacity for the Diagnostic and Management of CA in Africa
Considering the low task forces of trained specialists for CA in Africa, several approaches could be proposed [5]. The first thing should be to sensitize and train general practitioners for early recognition of cardiac arrhythmia. This is because Africa has gotten more general practitioners than cardiologists. These general practitioners (GPs) are often the first health professionals to manage CA in emergency units before specialized care by a cardiologist is taken cared of [9]. Secondly, general practitioners should also be trained in the initial management of severe cardiac arrhythmia before referral to a cardiologist. Algorithms for the management of severe cardiac arrhythmia should also be developed. These algorithms should be derived from available guidelines and adapted to the African context. General cardiologist should frequently take refresher courses on the diagnosis and management of cardiac arrhythmia, including basic knowledge of electronic devices such as pacemakers and intracardiac defibrillators. Finally, as widely practiced with good results in high-income countries, a system of e-consult should be put in place to contact specialists of cardiac arrhythmia in case of extreme emergencies with a patient having a dangered vital prognosis [10].
Simplified Approach for the General Practitioners in Africa
Given the complexity of CA for general practitioners, we propose a simplified strategy summarized in four steps to facilitate early recognition and management of CA in Africa.
Step 1: Suspect Cardiac Arrhythmia
Three mains clinicals signs should alarm general practitioners to clinically suspect cardiac arrhythmia: bradycardia < 50bpm, tachycardia > 120bpm and irregular heart beat [11-13].
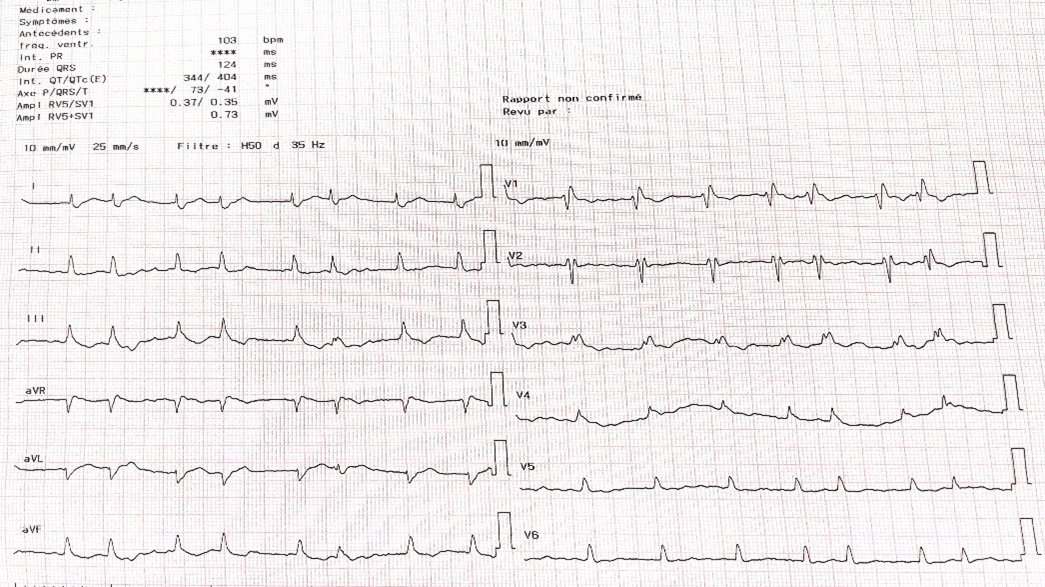
Figure 1: Absence of distinguished p wave with irregular QRS wave suggestive of atrial fibrillation.
Figure 2: Complete atrioventricular block with junctional escape rhythm (more p wave than QRS wave, regular PP and RR interval suggestive of atrioventricular dissociation).
Step 2: Confirm Cardiac Arrhythmia
If electocardiogram is available in the primary care setting, it should be done and send to a senior cardiologist or a trained specialist for cardiac arrhythmia to confirm the diagnosis of CA. Some features should be recognized by GPs even in absence of cardiologist: irregular rhythm without distinguished p wave is generally an ECG sign of atrial fibrillation (Figure 1); absence of p wave should indicated sino-atrial block; more p waves than QRS waves is a predictor of atrio-ventricular block (Figure 2). Tachycardia with non-enlarged QRS wave is a supraventricular tachycardia and tachycardia with an enlarged QRS wave generally suggest the diagnosis of ventricular tachycardia, except in some circumstances [11-13].
Step 3: Appreciate Severity
All type of cardiac arrhythmia should require urgent management if it is associated with thoracic pain, syncope or signs of congestive heart failure or hemodynamic instability such as a systolic blood pressure < 90mmhg, tachypnoea >20cpm, altered vigilance, pulselessness, cold extremity and cyanosis [11-13].
Step 4: Initial Management and Time for Referral
General practitioners should perform biological workups including serum electrolytes (especially kaliemia), complete blood count, renal function tests, C-reactive protein, activated cephalin time, thyroid function tests, prothrombin time, troponine level or natriuretic peptides if available. Imaging test to be performed include a chest X-ray and an echocardiogram [9]. In the absence of hemodynamic instability, advise on the continuity of treatment should be taken from a senior cardiologist for adequate management of CA. If the patient is hemodynamic unstable, early resuscitation therapy should be started. Here, resuscitation measures may include chest compressions ‘harder and faster’ in case of cardiac arrest and if available use external defibrillator (360 joules for monophasic and 150 joules for biphasic defibrillator), correction of electrolytes imbalance, oxygen supplement, fluid resuscitation in case of hypovolemic status, diuretics in case of congestive heart failure [9].
Specific treatment with atropine or isoprenaline (for complete heart block), adenosine (for junctional tachycardia), beta blockers (for supra-ventricular tachycardia) or amiodarone (for ventricular tachycardia) should be discussed with a consultant cardiologist or a specialist of cardiac arrhythmias [11-13]. In case of severe bradycardia, GPs could stop all negative chronotropes such as digoxin, beta blockers, verapamil and diltiazem. It is imperative to start vagal manoeuvres such as Valsalva for supraventricular tachycardia [9]. After initial management of hemodynamic instability, the patient should be addressed to a senior cardiologist or a specialist of cardiac arrhythmia for specific management.
Conclusion
Cardiac Arrhythmia is an emerging cause of death in Africa. As there is a low task force of specialist in this continent. Capacity building by training general practitioners to better diagnose and manage of this condition in Africa appears to be a promising way forward in curbing the huge burden of CA in this third-world continent.
Conflicts of Interest
None.
Author Contributions
Conception of the study: MNT; Manuscript writing: MNT; Critical revision: All the authors.
Funding
None.
Abbreviations
AF: Atrial Fibrillation
CA: Cardiac Arrhythmia
GP: General Practitioners
LMICs: Low-and Middle-Income Countries
WHF: World Heart Federation
Article Info
Article Type
Review ArticlePublication history
Received: Sat 02, Jan 2021Accepted: Thu 14, Jan 2021
Published: Mon 25, Jan 2021
Copyright
© 2023 Mazou N Temgoua. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2021.01.08
Author Info
Mazou N Temgoua Jérôme Boombhi Joel Noutakdie Tochie Amalia Owona Samuel Kingue
Corresponding Author
Mazou N TemgouaDepartment of Internal Medicine and Specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaoundé, Cameroon
Figures & Tables

References
- Paratz ED, Rowsell L, Zentner D, Parsons S, Morgan N et al. (2020) Cardiac arrest and sudden cardiac death registries: a systematic review of global coverage. Open Heart 7: e001195. [Crossref]
- Khurshid S, Choi SH, Weng LC, Wang EY, Trinquart L et al. (2018) Frequency of Cardiac Rhythm Abnormalities in a Half Million Adults. Circ Arrhythm Electrophysiol 11: e006273. [Crossref]
- Mkoko P, Bahiru E, Ajijola OA, Bonny A, Chin A (2020) Cardiac arrhythmias in low- and middle-income countries. Cardiovasc Diagn Ther 10: 350‑360. [Crossref]
- Yuyun MF, Bonny A, Ng GA, Sliwa K, Kengne AP et al. (2020) A Systematic Review of the Spectrum of Cardiac Arrhythmias in Sub-Saharan Africa. Glob Heart 15: 37. [Crossref]
- Bonny A, Ngantcha M, Scholtz W, Chin A, Nel G et al. (2019) Cardiac Arrhythmias in Africa: Epidemiology, Management Challenges, and Perspectives. J Am Coll Cardiol 73: 100‑109. [Crossref]
- Bonny A, Ngantcha M, Jeilan M, Okello E, Kaviraj B et al. (2018) Statistics on the use of cardiac electronic devices and interventional electrophysiological procedures in Africa from 2011 to 2016: report of the Pan African Society of Cardiology (PASCAR) Cardiac Arrhythmias and Pacing Task Forces. Europace 20: 1513‑1526. [Crossref]
- Murphy A, Banerjee A, Breithardt G, Camm AJ, Commerford P et al. (2017) The World Heart Federation Roadmap for Nonvalvular Atrial Fibrillation. Glob Heart 12: 273‑284. [Crossref]
- Amegah AK (2018) Tackling the Growing Burden of Cardiovascular Diseases in Sub-Saharan Africa. Circulation 138: 2449‑2451. [Crossref]
- Cruickshank J (2008) Initial management of cardiac arrhythmias. Aust Fam Physician 37: 516-520. [Crossref]
- Kim EJ, Orlander JD, Afable M, Pawar S, Cutrona SL et al. (2019) Cardiology electronic consultation (e-consult) use by primary care providers at VA medical centres in New England. J Telemed Telecare 25: 370‑377. [Crossref]
- Al Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ et al. (2018) 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Circulation 138: e272‑e391. [Crossref]
- Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA et al. (2019) 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 74: 932-987. [Crossref]
- Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ et al. (2020) 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J 41: 655-720. [Crossref]
