A Surprising Finding of Ileal Intussusception Caused by Pleural Mesothelioma Metastases
A B S T R A C T
Background: Malignant pleural mesothelioma is an aggressive form of cancer originating in the pleural mesothelioma. It generally appears as a local disease in the affected hemithorax, and metastasis are rare. It is unusual for malignant pleural mesothelioma to manifest with gastrointestinal complications due to metastatic implants, but clinicians should be careful to take into consideration this hypothesis in patients with a history of malignant pleural mesothelioma referring to the Emergency Department with acute abdominal pain.
Case Presentation: A 65-year-old man, with a medical history of pleural mesothelioma, presented to our emergency department for acute abdominal pain. The patient underwent abdominal ultrasound and abdominal Computed Tomography with intravenous contrast. At US examination a small bowel obstruction diagnosis was made, CT confirmed a mechanical small bowel obstruction due to an intussuscepted multiloculated mass in the terminal ileum, with CT’s signs of parietal damage; another peritoneal mass was reported adjacent to the posterior wall of the cecum and in contiguity with the iliopsoas muscle. Considering the acute medical presentation, the patient underwent surgery, with segmental bowel resection and a stapled side-by-side bowel anastomosis. Histopathology revealed metastasis of sarcomatoid pleural mesothelioma. The post-operative course was complicated by anastomotic leak treated with a conservative approach. The patient was discharged on the 24th post-operative day.
Conclusion: Our case highlights the potential of pleural mesothelioma to metastasize within abdominal viscera, causing bowel obstruction. In presence of the patient’s critical clinical condition and advanced state of local disease, a surgical approach based on damage control procedure consisting in exploration, biopsies and ileostomy upstream the obstruction or, exploration and resection without anastomosis, carry on several advantages, solving the acute clinical condition, staging the disease and offering the possibility to proceed rapidly with supportive care (chemotherapy and/or surgery).
Keywords
Malignant pleural mesothelioma, small bowel obstruction, small bowel intussusception
Background
Mesothelioma is a rare neoplasm originating from cells of the serosal cavities, and approximately 90-95% of mesotheliomas arise in the pleural cavity. The typical symptoms include chest pain, dyspnea, unexplained unilateral pleural effusion, or other nonspecific respiratory symptoms. It is characterized by aggressive local-regional invasion due to its direct extension through the hemidiaphragm and/or hematological spread [1]. Frequently metastasis involves regional lymph nodes, contralateral lung, liver, adrenal glands and kidney; isolated involvement of the gastrointestinal lumen is extremely rare. There are only five cases of malignant mesothelioma with gastrointestinal involvement reported in previously published studies [2]. In these patients, gastrointestinal and peritoneal implants may cause bowel obstruction with or without perforation and sometimes bleeding [3, 4]. Clinicians should be careful to take into consideration this diagnostic hypothesis in patients with a history of malignant pleural mesothelioma referring to the Emergency Department with acute abdominal pain. We present a case of a man who presented at our emergency department with acute abdominal pain and symptoms of bowel obstruction due to intussusception caused by endoluminal metastasis of sarcomatoid pleura mesothelioma in the terminal ileum.
Case Presentation
A 65-year-old man, with a medical history of pleural mesothelioma, in chemotherapy treatment with platinum and folate, referred at our hospital for acute abdominal pain, he had not been evacuating for three days. The physical abdominal examination showed abdominal distension and pain in the lower right quadrant. Laboratory tests showed leukocytosis (22,000/mm3), increased C reactive protein value, and reduced Hb value (Hb 8,4 g/dl). The patient underwent an abdominal ultrasound that showed free fluid between bowel loops, dilated small bowel loops (outer wall to outer wall diameter > 2.5 cm) and bowel hypocinesis; endoluminal soft tissue mass with a donut morphology resembling an ileocolic intussusception was detected, and a suspected diagnosis of small bowel obstruction caused by intussusception was made [5]. The patient underwent contrast-enhanced abdominal computed tomography (CT) that confirmed the US’s diagnosis of mechanical bowel obstruction; a soft tissue mass of (37x24x36 mm, DTxDLxDAP) was detected in the lumen of the terminal ileum, the endoluminal lesion presented irregular and lobulated margins, cerebroid aspect and inhomogeneous contrast enhancement.
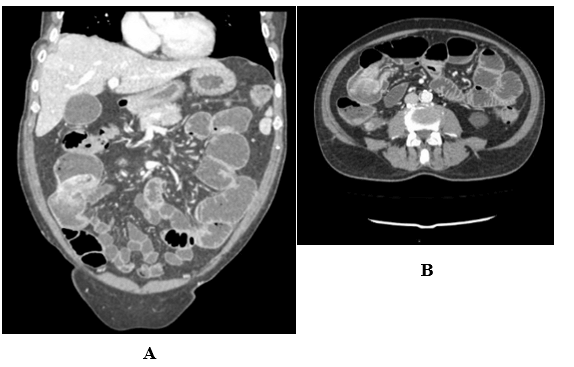
Another solid lesion with irregular margins was detected between the right colon and iliopsoas muscles. CT findings suggested a mechanical obstruction due to intussuscepted malignant mass in the terminal ileum acting as lead point; reported lesions were referred as “probably metastatic”, given the patient’s history (Figures 1A & 1B) [6]. An emergency surgical approach was performed, due to acute medical presentation, hemodynamic instability, increased heart rate (HR> 120 bpm), reduced blood pressure (systolic pressure< 100 mmHg) and significantly reduced Hb value, in association with the radiological examination of mechanical small bowel obstruction due to an intussuscepted solid mass within terminal ileum.
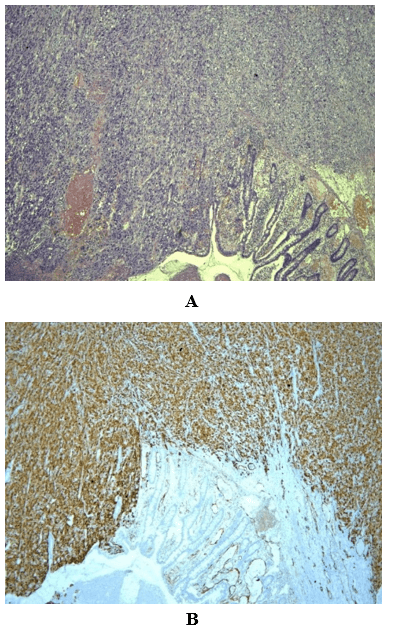
During the exploration of the abdominal cavity, the small bowel was significantly dilated, with extremely thin layers and parietal perfusions alterations, with no evidence of necrosis. Free fluid between bowel loops was detected, and the mass within the intussuscepted terminal ileum was confirmed (localized at 80 cm from ileocecal valve), acting as the leading point in the mechanical obstruction. The mass was excised with the help of a segmental bowel resection and a stapled side-by-side bowel anastomosis. Histopathological examination with positive immunohistochemical for WT1 protein and 29hD1 calbindin and high proliferative index (ki67 positive >70%) confirmed a sarcomatoid metastasis of pleural mesothelioma. (Figures 2A & 2B). The post-operative course was regular at the beginning, while during the 6th post-operative day, it was complicated by anastomotic leak treated conservatively treated with naso-gastric decompression, IV fluids, and bowel rest [7]. The patient was discharged on the 24th post-operative day and underwent adjuvant chemotherapy.
Figures 1: CT with iv contrast. A) Coronal MPR: fluid-filled small bowel loops, in the lumen of the terminal ileum, presence of an irregular lesion with lobulated margins, cerebroid aspect, and inhomogeneous contrast enhancement. B) Another solid lesion with irregular margins was detected between the right colon and iliopsoas muscles.
Figures 2: A) Hematoxylin and eosin-stained section revealed metastasis involving ileal wall extrinsic, the mucosae are negative.B) Immunohistochemical diagnosis of mesothelioma with positivity to WT1 protein.
Discussion
The intra-abdominal involvement of pleural mesothelioma can be the result of direct extension through the hemidiaphragm or to “spilling” of mesothelioma cells into the peritoneal cavity in the post-operative course of resected primitive tumor adjacent to the diaphragm [1, 4]. The distant metastases for hematogenous or lymphatic spread are rare [3, 4, 8-12]. Sugarbaker et al. reported a group of patients presenting with acute onset of abdominal pain due to perforation or obstruction of gastrointestinal caused by gastrointestinal metastases, who underwent surgical intervention in emergency settings [13]. The aim of our study was to highlight the potential of pleural mesothelioma abdominal metastasis to cause mechanical small bowel obstruction, and moreover, to offer our experience to the surgeons in order to pay particular attention to these kinds of patients.
Theoretically, a surgical approach based on damage control procedure consisting of exploration, biopsies and ileostomy upstream the obstruction, or exploration and resection without anastomosis, would let the surgeon to perform a “second look” in favor of a more radical surgical resection in emergency settings. This attitude would carry on several advantages, at first solving the acute clinical condition, then getting a diagnosis and the staging of the disease and helping the patient to start a second line of therapy (chemotherapy and/or surgery) with reduced risks of complications rapidly.
In our case, although there were indications to perform an emergency surgical approach (segmental bowel resection and bowel anastomosis) in order to solve the acute medical presentation, a different and less invasive approach (debulking therapy) was not supported by patient’s critical clinical condition and the severe obstruction due to the advanced stage of local disease. As a matter of fact, in a retrospective analysis of our approach, the choice to perform the anastomosis in the emergency settings still looks questionable, confirmed by the fact that the patient presented with anastomosis leakage and sequently a self-resolving fistula (Clavien Dindo II). Although complications resolved with conservative therapy, fistula prejudiced hereinafter the systemic therapy, with the risk of a possibly rapid progression of disease in chest area. Our case highlights two major points: first of all, the possibility of acute gastrointestinal syndromes in patients with malignant mesothelioma metastasis and that a damage control procedure should be the first approach.
Article Info
Article Type
Case ReportPublication history
Received: Fri 24, Apr 2020Accepted: Wed 13, May 2020
Published: Sat 16, May 2020
Copyright
© 2023 Stefania Tamburrini. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.05.09
Author Info
Antonella Pesce Ester Marra Giuseppe Mercogliano Giuseppe Militerno Giuseppe Iannacci Ines Marano Maria Luisa D’Aponte Pasquale Tammaro Pietro Maida Stefania Tamburrini
Corresponding Author
Stefania TamburriniDepartment of Radiology, Ospedale del Mare, ASL NA1 Centro, Naples, Italy
Figures & Tables
References
- Tsao AS, Wistuba I, Roth JA, Kindler HL (2009) Malignant pleural mesothelioma. J Clin Oncol 27: 2081-2090. [Crossref]
- Chen JH, Huang TC, Chang PY, Dai MS, Ho CL et al. (2014) Malignat bowel obstruction: A retrospective clinical analysis. Mol Clin Oncol 2: 13-18. [Crossref]
- Chen HC, Tsai KB, Wang CS, Hsieh TJ, Hsu JS (2008) Duodenal metastasis of malignant pleural mesothelioma. J Formos Med Assoc 107: 961-964. [Crossref]
- Tertemiz KC, Ozgen Alpaydin A, Gurel D, Savas R, Gulcu A et al. (2014) Multiple distant metastases in a case of malignant pleural mesothelioma. Respir Med Case Rep 13: 16-18. [Crossref]
- Tamburrini S, Lugara M, Iaselli F, Saturnino PP, Liguori C et al. (2019) Diagnostic Accuracy of Ultrasound in the Diagnosis of Small Bowel Obstruction. Diagnostics (Basel) 9. [Crossref]
- Somma F, Faggian A, Serra N, Gatta G, Iacobellis F et al. (2015) Bowel intussusceptions in adults: the role of imaging. Radiol Med 120: 105-117. [Crossref]
- Thaker DA, Stafford BC, Gaffney LS (2010) Palliative management of malignant bowel obstruction in terminally ill patient. Indian J Palliat Care 16: 97-100. [Crossref]
- Lin YT, Wu BS, Yang SF, Chen HC (2009) Isolated pancreatic metastasis of a malignant pleural mesothelioma. Kaohsiung J Med Sci 25: 395-400. [Crossref]
- Gocho K, Isobe K, Kaburaki K, Honda Y, Mitsuda A et al. (2010) Malignant pleural mesothelioma presenting as an acute surgical abdomen due to metastatic jejunal perforation. Intern Med 49: 597-601. [Crossref]
- Sibio S, Sammartino P, Accarpio F, Biacchi D, Cornali T et al. (2011) Metastasis of pleural mesothelioma presenting as bleeding colonic polyp. Ann Thorac Surg 92: 1898-1901. [Crossref]
- Falkenstern Ge RF, Kimmich M, Bode Erdmann S, Friedel G, Ott G et al. (2013) Pleural mesothelioma presenting as periumbilical metastasis: the first clinical documentation. Case Rep Oncol Med 2013: 198729. [Crossref]
- Navarro García MI, Sánchez Pérez A, Vázquez Rojas JL (2015) Jejunal Perforation by Metastasis of Malignant Pleural Mesothelioma. Arch Bronconeumol 51: 366-367. [Crossref]
- Sugarbaker PH (2017) Intra-abdominal manifestations of pleural mesothelioma. Ann Transl Med 5: 231. [Crossref]
