A Chronic Non-Healing Oral Lesion in a Breast Cancer Patient
A B S T R A C T
This case report takes readers through our journey to a diagnosis of a breast cancer metastasis superimposed on a stage II MRONJ lesion. It highlights the importance of sending all bone sequestra excised intraoperatively for histopathological examination.
Keywords
Medication-related osteonecrosis of the jaw, breast cancer, metastasis, metastatic disease to the mandible
Clinical Presentation
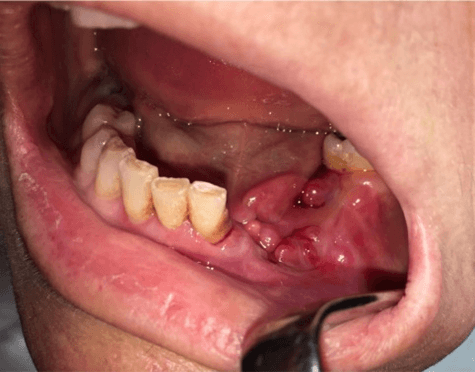
A 61-year-old female was referred to the department of Oral and Maxillofacial Surgery with a non-healing oral lesion from a private dental practice. In April 2018, she had undergone extraction of tooth 34 (lower left 1st premolar). The socket did not heal (Figure 1), so she underwent two revisions, as well as a subsequent deep-cleaning and treatment of tooth 35 before being referred to our department in August 2018. She suffered intense, persistent pain of a VAS magnitude of 8/10. The patient had been diagnosed with breast cancer in 2003, for which she had a double mastectomy and hysterectomy in 2004 and was on Ibandronate from 2012 for metastases to her thoracic vertebrae. Tumor markers were mildly elevated, but PET/CT did not reveal any active lesions. The patient had previously undergone radiotherapy to her axilla and the presentation was between courses of chemotherapy, which had resulted in the development of reactive thrombocytopenia.
Figure 1: Appearance at four weeks post-extraction of tooth 34.
Intraoral examination revealed a periosteal reaction and both buccal and lingual fistulae in the region of teeth 33-35 (Figure 2). There was wound dehiscence around the extraction site of tooth 34. Tooth 32 had grade 1 mobility, 33 had grade 3 mobility, and 35 was firmly attached. Extraoral examination showed mild swelling around the region of the mandible and she had paraesthesia affecting the left side of her chin. Imaging in the form of an OPG revealed changes to the structure of the bone in the region 32-34. Cone-beam computed tomography was done to more accurately define the extent of the lesion (Figure 3).
Figure 2: Oral examination revealed erythema, swelling, and vestibular and lingual fistulae in the region of 33-35.
Figure 3: CBCT showing the destruction of the bone in the region 33-34.
I Differential Diagnosis
The patient was on Ibandronate- an anti-resorptive medication, to prevent metastases of her breast cancer. One rare side effect of anti-resorptive medications is Medication-Related Osteonecrosis of the Jaw (MRONJ), defined by the American Association of Oral and Maxillofacial Surgeons as a lesion with “exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for longer than 8 weeks” [1]. Although the patient met the criteria for MRONJ, the fact that bone was not fully exposed (merely accessible via fistulae) opened up a wider range of possible aetiologies. These differential diagnoses include conditions such as osteoradionecrosis, metastatic or primary bone tumors, and (infective) osteomyelitis [2].
Osteoradionecrosis (ORN) of the jaw is virtually indistinguishable, both clinically and radiologically, from MRONJ but it is an etiologically separate condition altogether [1]. We ruled out ORN in this case, as the patient had not received radiotherapy to the head or neck, but only to the axilla and it was unlikely that scatter radiation from this would lead to ORN. Other possible differential diagnoses of conditions arising after tooth extraction that present with non-healing, like alveolar osteitis (dry socket) were also excluded. The patient did not suffer from symptoms immediately post-extraction, and additionally, she was not a smoker, diabetic, or taking the OCP/HRT. Though she was arguably immunosuppressed from her chemotherapy, osteitis was ruled out as being unlikely to be the cause. Being an oncology patient, tumor metastasis was a distinct possibility. It is well-established that up to 75% of breast cancer patients with metastatic disease will have involvement of the bony skeleton [3]. However, it is considered quite rare for metastatic spread to involve the jaws, as only about 1% of cases do [4].
Alternatively, the patient may have also developed another primary tumor. Compared to the general population, cancer sufferers are at a statistically higher risk of developing other malignancies. In fact, multiple primary neoplasms are common oncological findings. Whether this is due to repeated bouts of immunosuppression from multiple cycles of chemotherapy, the direct toxic effects of the chemo- and radiotherapies themselves or whether it is simply a consequence of stress and ageing, remains unclear [5]. Osteomyelitis (inflammation of bone parenchyma that typically develops as a consequence of infection) of the jaws following dental procedures is a rare condition, which may be associated with the use of drugs such as corticosteroids and chemotherapeutic agents [6]. Our patient had been treated with the cytotoxic Vinorelbine, as well as the cyclin-dependent kinase inhibitor Abemaciclib, which had been associated with leukopenia [7]. However, according to her blood count, the patient was not leukopenic (her WBC was at the lower end of the range but still normal) and osteomyelitis usually develops in the context of immune suppression. She did have a raised immature granulocyte count; however, this could indicate any form of infection or another form of inflammation and could have been a consequence of the non-healing lesion itself. The overall clinical presentation and imaging results indicated a diagnosis of MRONJ.
Figure 4: Basic staining with hematoxylin-eosin (H&E): a) Desmoplastic tissue sample (pink tissue), groups of small dark cells in the center of the image are tumorous (x40); b) higher magnification (x400) showing details of tumor cells.
II Diagnosis
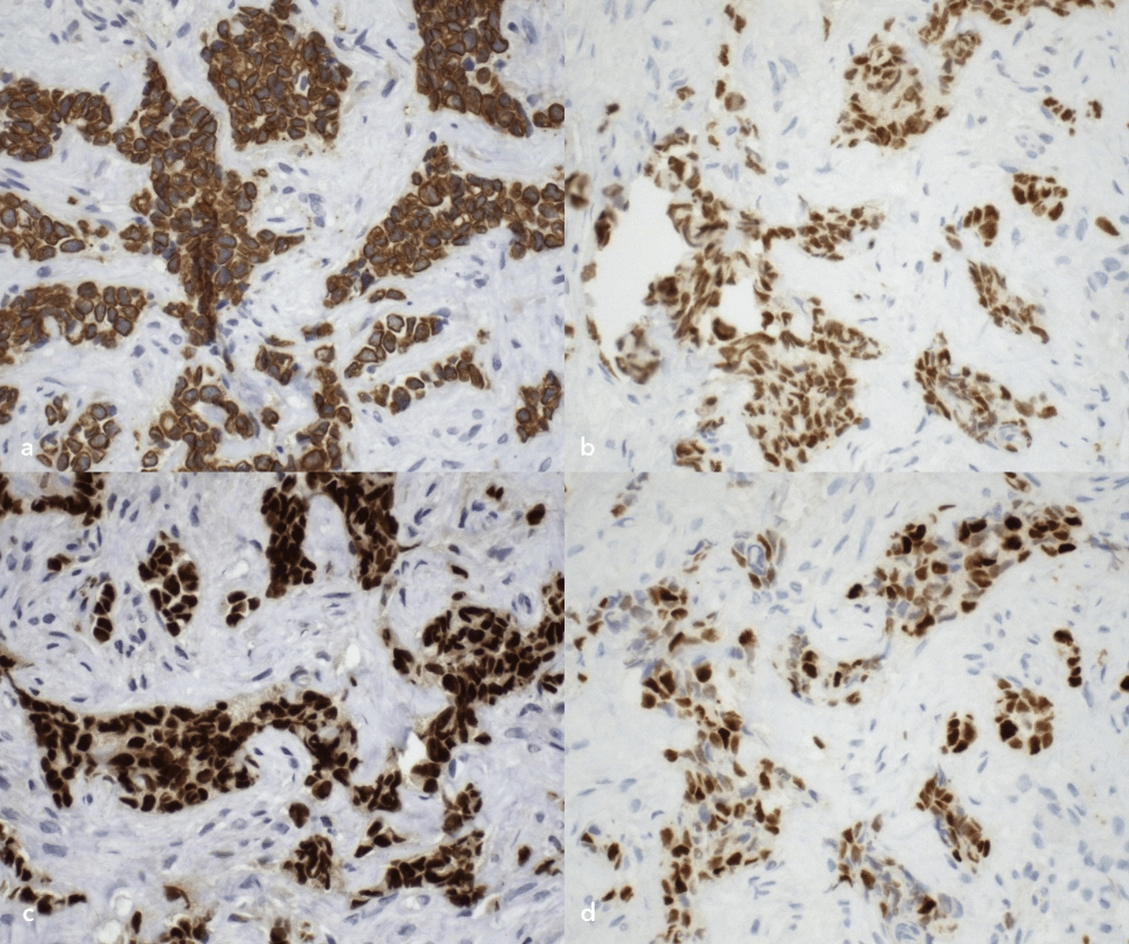
Thus, under the working diagnosis of MRONJ, a sequestrectomy was performed. However, histopathological findings of the removed necrotic tissue revealed that the region 33, the part of the sequestrum contained infiltration by atypical cells (Figure 4), which, using immunohistochemistry, were determined to be carcinoma of the breast (CKAE1-3, GATA 3, ER, PR- positive) (Figure 5). Thereby, the final diagnosis was amended to a case of a breast cancer metastasis superimposed on a stage II MRONJ lesion.
Figure 5: Immunohistochemical examination. a) Staining for general cytokeratins (CKAE1-3): brown cytoplasmic positivity of the tumorous cells demonstrates their epithelial origin. b-d) Staining for hormonal receptors GATA3, ER, and PR, respectively: brown nuclear positivity; in this case, positivity for all of these markers is proof that the origin of the cells is from breast tissue.
III Management
The first part of the management was the sequestrectomy that led to obtaining the histopathological sample. In fact, at the time of the operation, it was believed that this intervention would be the main component of her treatment for MRONJ. The patient was admitted for sequestrectomy under local anaesthesia. In light of the existing thrombocytopenia, the procedure was done primarily with the aim of eliminating the patient’s pain, removing the necrotic tissue, and extracting the affected teeth. The mucoperiosteum was retracted to reveal the necrotic bone. Since the necrotic tissue extended to below the teeth 32 and 35, they were both also extracted. The sequestrum in the region 33 was removed along with several millilitres of pus and the area was thoroughly debrided. All removed tissue was sent for histological examination. The wound was cleaned using a combination of H2O2 and Betadine, then local haemostatic agents were applied and the site was sutured and closed, obtaining full mucosal coverage. On the basis of the subsequent histopathological findings, the patient was referred for palliative radiotherapy of the affected jaw to treat the breast cancer metastasis. Unfortunately, the patient died a short time after the diagnosis. Therefore, we were not able to establish her response to the treatment.
Discussion
Osteonecrosis of the Jaw develops as a consequence of bone metabolism being altered by medications, such as Bisphosphonates, Denosumab (antiresorptive) or Sunitinib (an antiangiogenic). Patients are typically placed on antiresorptive therapy in an effort to decrease the incidence of skeletal-related events (SREs) associated with metastatic bone disease or to reduce the risk of pathological fractures in osteoporosis [1]. As mentioned above, only about 1% of metastases involve the jaw bones. Additionally, it is quite rare for metastasis to be superimposed upon another pathology. Of the cases that do metastasize to the jaws, the mandible is more commonly affected than the maxilla [8]. Breast and prostate carcinomas are the malignancies most likely to metastasize to the oral cavity [9]. This patient is the first case of MRONJ-associated metastasis to the jaw that we have encountered in our department, where we have dealt with over 350 cases of MRONJ over the past 12 years. Approximately 30% of our MRONJ patients have breast cancer. We believe that this case highlights the importance of sending all bone sequestra excised intraoperatively for histopathological examination, as, like in this case, it may actually be hiding another disease process.
Conflicts of Interest
None.
Ethics Statement
Patient permission for the use of clinical photographs for publication in medical journals was obtained. Ethics board of approval not required.
Article Info
Article Type
Case ReportPublication history
Received: Thu 04, Feb 2021Accepted: Thu 18, Feb 2021
Published: Thu 04, Mar 2021
Copyright
© 2023 Anna Onderková. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.03.02
Author Info
Anna Onderková Nima Mahdian Eitan Brizman Jana Rosmusová Gabriela Vajchrová Gabriela Pavlikova
Corresponding Author
Anna OnderkováOral & Maxillofacial Surgery Department, VFN, General University Hospital & Charles University, 1st Faculty of Medicine, Prague, Czech Republic
Figures & Tables



References
1.
Ruggiero,
Salvatore L, et al. (2014) American Association of Oral and Maxillofacial
Surgeons position paper on medication-related osteonecrosis of the jaw--2014
update. J Oral Maxillofac Surg 72: 1938-1956. [Crossref]
2.
Gupta M, Gupta N
(2020) Bisphosphonate Related Jaw Osteonecrosis. StatPearls [Internet].
[Crossref]
3.
Harvey HA, Cream
LR (2007) Biology of bone metastases: causes and consequences. Clin Breast
Cancer 7: S7-S13. [Crossref]
4.
Hirshberg A,
Berger R, Allon I, Kaplan I et al. (2014) Metastatic tumors to the jaws and
mouth. Head Neck Pathol 8: 463-474. [Crossref]
5.
Koubková L,
Hrstka R, Dobes P, Vojtesek B, Vyzula R (2014) Second primary cancers -
causes, incidence and the future. Klin Onkol 27: 11-17. [Crossref]
6. Nezafati S, Ghavimi MA, Yavari AS (2009) Localized osteomyelitis of the mandible secondary to dental treatment: report of a case. J Dental Res Dent Clin Dent Prospect 3: 67-69. [Crossref]
7.
McCartney A, Moretti
E, Sanna G, Pestrin M, Risi E et al. (2018) The role of abemaciclib in
treatment of advanced breast cancer. Ther Adv Med Oncol 10:
175883591877692. [Crossref]
8.
Hirshberg A,
Leibovich P, Buchner A (1994) Metastatic tumors to the jawbones: analysis of
390 cases. J Oral Pathol Med 23: 337-341. [Crossref]
9.
Hirshberg A, Shnaiderman Shapiro A, Kaplan I, Berger R
(2008) Metastatic tumours to the oral cavity—pathogenesis and analysis of 673
cases. Oral Oncol 44: 743-752. [Crossref]
